Two Cysts Around the Knee
Hear From Our Patients
Patient Experience Partial Meniscectomy for Meniscus Tear & Baker's CystSwelling around the knee is problematic. Swelling behind the knee is often called a Baker’s cyst while swelling at the side of the knee is usually a meniscus cyst. The commonality is that both originate from a meniscus injury. Here is their story.
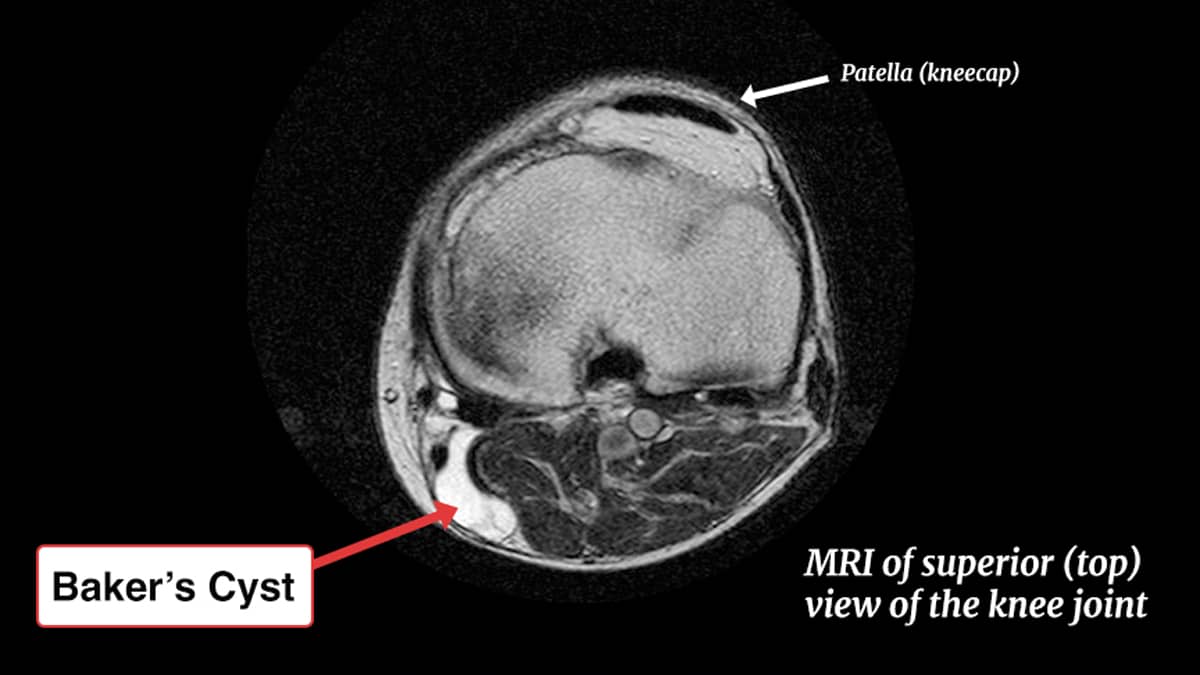
Baker was a 19th-century surgeon who correctly identified the cysts at the back of the knee as related to an injury to the meniscus—most commonly (and sometimes solely) from arthritis. Damage inside the knee irritates the lining cells of the synovium (the wall of the knee joint) and those cells generate excess fluid. This fluid often tracks to the back of the knee joint, forming a pouch. Over time, the pouch develops a thickened layer, preventing the fluid from being absorbed. In some cases, the cysts form multiple pouches; this is called a multilobulated cyst. Our research, and that of others, has used MRI scanning to determine that 80% of the time Baker’s cysts originate from a meniscus tear in the posterior quarter of the meniscus.
The Baker’s cyst rarely resolves on its own. Aspirating the fluid and adding steroids is a temporizing measure. Definitive therapy requires that we surgically excise the cyst and repair the meniscus tear itself or treat the underlying arthritis so effectively that the repetitive stimulus causing excess joint fluid is resolved. If this is not done, the cysts may get large and even rupture, causing concern for a blood clot and calf pain.
Meniscus cysts are slightly different. Most commonly originating from the lateral meniscus, a tract is formed to the side of the knee. On an MRI, the meniscus looks degenerated, with fluid within the collagen fibers and a small outcropping to the side of the joint. Since the skin and ligaments are generally tight in this area, any small amount of swelling produces noticeable pressure.
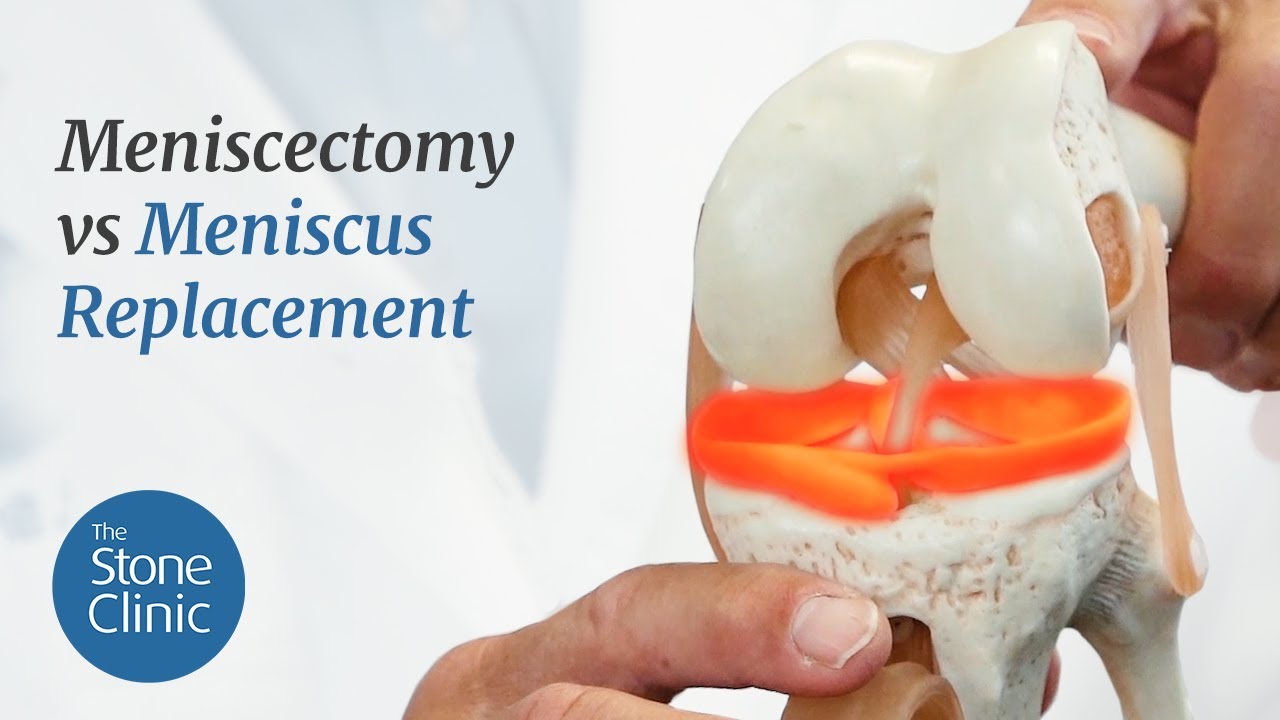
The degenerated lateral meniscus is difficult but not impossible to repair. First, the damaged tissue inside the meniscus must be shaved away with the cyst walls. Suture repair is then possible, often augmented by PRP or bone marrow release to stimulate a more potent healing response. Unfortunately, meniscus repair in cystic menisci has a high failure rate. The salvage strategy is to replace the tissue with a donor meniscus.
Unlike Baker—who might have removed the entire meniscus when a cyst was present, dooming the knee to progressive arthritis—today’s surgeons can repair the causes, remove the cysts, and preserve the precious days of a patient’s athletic life.