My Lessons from the 2023 ACL Study Group Meeting
The ACL Study Group is a biannual meeting of select ACL surgeons who gather from around the world to discuss the latest knowledge in ACL treatment. Here are a few of the lessons from the 2023 meeting.
ACL injury risk is still far too high in soccer, basketball, football, rugby, and skiing. Forty-five percent of the 2022 US Women’s National Soccer team had ACL injuries(1). A skier attempting to race on the World Cup circuit will likely suffer three near career-ending knee injuries between their youth and their racing career. These ACL injuries are relatively devastating to the professional careers of most athletes. Even though they return to sport after reconstruction, it takes two years to get back to their previous level and shortens most professional careers significantly.
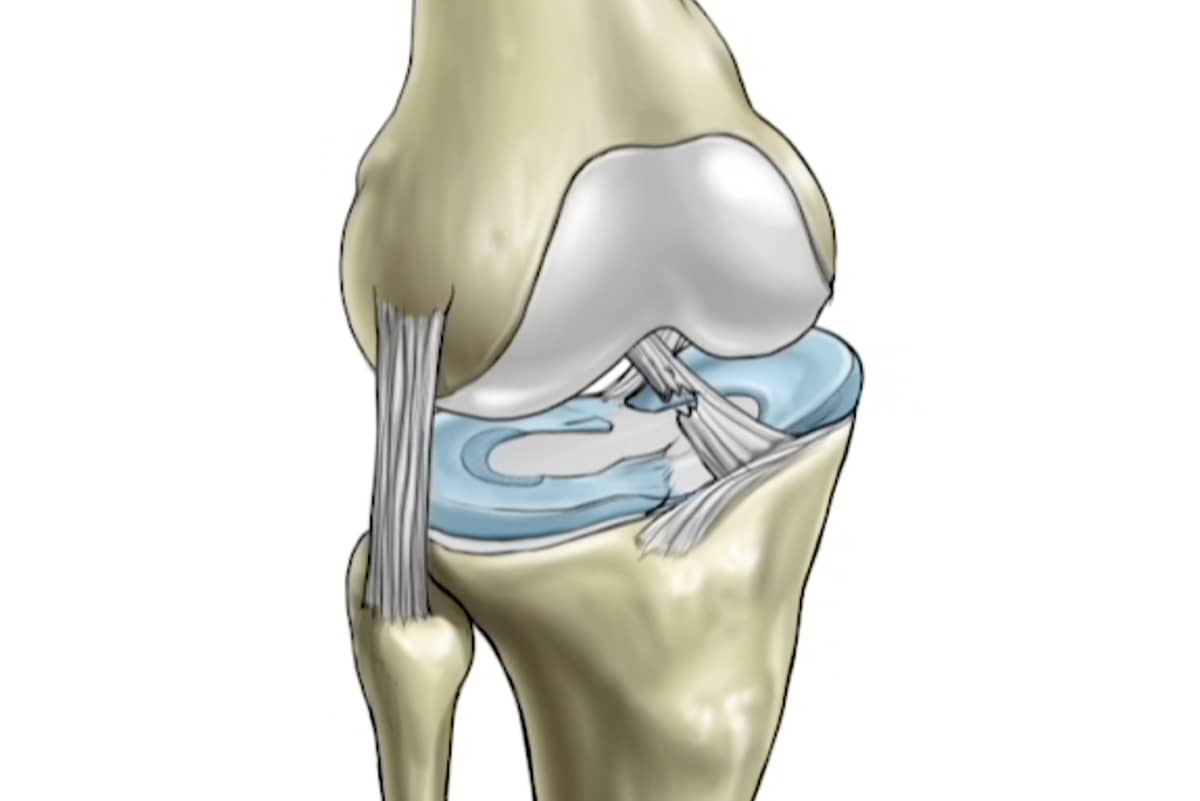
Many of the problems encountered in 2023 are the same ones that have been studied for decades—especially the fact that, when the ACL is injured, other tissues in the knee are injured and must be repaired as well (especially the meniscus and articular cartilage). Failure to restore those tissues dooms the knee to arthritis.
Other issues include the choice of tissue used for repair. The patient’s own hamstrings, patellar tendon, or quadriceps tendons all seem to have relatively high success rates at returning the knee to stability. Even with their use, there is still a recurrence rate up to 30% in high-level athletes and usually around 4% to 15% in everyone else. The use of allografts (donor tissues), meanwhile, has evolved. We now use only fresh-frozen (not irradiated) young, healthy tissue, often from the thicker quadriceps tendon. The use of allografts remains limited by low availability in many countries and by the higher re-rupture rate reported from earlier experience. A parent of a child has an especially difficult choice as they must still choose between the use of donor tissue—which may have a higher chance of re-rupture—or the harvesting of the patient’s own tissues, which still has an uncomfortably high re-tear rate and is also associated with permanent weakness and arthritis.
There is no evidence of a higher rupture rate in athletes over the age of 25 when donor tissues are used and no definitive data yet demonstrating better outcomes using the younger, better donor tissues. There is convincing data, however, that using the patient’s own hamstrings leads to permanent loss of motor power while taking the patellar tendon to reconstruct the patient’s own ACL is associated with a high incidence of anterior knee arthritis(3).
To date, no artificial ligaments have worked. Xenografts remain in the research stage after a successful pilot study in the US (but an unfortunate manufacturing contamination in a wide clinical trial in Europe). They are likely to return.
Another point of discussion at the meeting was that surgical technique matters. Accurate placement of the substitute grafts into the anatomic sites of the native ACL is crucial to a successful outcome. Vertical grafts or anteriorly placed grafts do not stabilize the knee properly and are a common cause of revision surgery. Fixation of the grafts is now excellent, with a wide range of techniques.
Robots, using advanced AI, are coming. They will be used both to examine the knee in order to get an accurate assessment of which tissues are injured and how much laxity exists in the knee’s rotation and flexion and to assist during repair of the knee by ensuring accurate tunnel placement. While still in the testing phase, the hope is that robots—given the large number of misdiagnoses and misplaced ACLs in the community—may soon provide solutions to those problems.
Surgical augmentation of the lateral or outside part of the knee called anterior lateral ligament reconstruction (ALL), iliotibial band tenodesis, lateral extraarticular tenodesis (LET), and posterolateral corner reconstruction (PLC) all significantly reduce the incidence of failed ACL reconstruction. In a group of professional soccer players the failure rate was reduced to 2% by the combination of ACL reconstruction plus LET(2). The extraarticular surgery may work by repairing an injured structure or simply by protecting the ACL during the healing window. Either way, far more primary ACL reconstructions are being augmented by a lateral procedure and almost all revisions performed by the top ACL surgeons are being backed up by lateral grafts.
Can the ACL be reliably repaired rather than replaced after injury? ACL repair, with or without collagen devices or internal braces, remains a controversial space. There is a general belief that only a few ACL injuries, with very high partial tears in older people, are the ideal candidates. Some recent data in younger patients is encouraging—though previous ACL repair studies have noted that while the repairs looked good at two years, they generally failed after five years. So the answer to this question is not yet in.
Early complete range of motion is a critical factor in successful patient outcomes. Range of motion, it turns out, is far more important than regaining strength in the early post-operative period. New data evaluating the connection between the brain, the hip, and the muscles of the knee demonstrate that the early hamstring muscle tension leads to loss of extension, but can be overcome by prone exercises, physical therapy, massage, and release of the muscle tension causing the loss of motion(4).
All knees, after injury, develop an inflammatory response to initiate the healing process. Normally, this elevation in inflammatory cells recruits macrophage cells that race to the site of injury and then shift from the inflammatory stage M1 cells to the healing stage M2 cells. There are specific growth factors and mediators that help that switch occur. Some people, however, remain in the inflammatory stage. These people must postpone surgery until the knee quiets down. New injections, and possibly oral medications and supplements, may actually help the M1 cells switch from pro-inflammatory to the anabolic healing environment of M2 cells. These special pro-resolving mediators (SPMs) are the subject of intense research and development.
The addition of PRP, stem-cell-recruitment factors, lubrication, and inflammation modulators is currently a hot area of research. These factors may soon be applied to all knee injuries to guide their course to successful healing.
Preventive exercise programs continue to show significant benefits in reducing the number of ACL injuries in athletes and teams who commit to these programs before the seasons begin. They include not just the training of the quads and hamstrings, but also the training of the brain/body connection—especially the hip, knee, and ankle position when landing. A disconnection of this relationship, even momentarily, leads to the sudden overloading of the knee ligaments. But despite the overwhelming data that ACL injury prevention programs work, compliance with the programs is distressingly low. It could be that, just as you must pass a test to get your driver’s license, you should probably be required to pass an ACL injury prevention course annually to play on an ACL injury-producing team. One counterargument to this is that these courses do not work for everyone—and there is no universal athlete preinjury identification technique.
ACL reconstruction surgery works for most patients, returning them to sports with stable knees and hopefully reducing the rate of new injury to the meniscus and articular cartilage. Yet there is room for substantial improvement at every stage—from prevention, surgery, and anabolic stimulation to rehabilitation. This creates a spectacular opportunity for young scientists, physicians, surgeons, trainers, and rehabilitation specialists to make enormous contributions to the world. Come join us!
References:

