Biologic Injections
Hear From Our Patients
Running Pain Free After Knee PRP InjectionsInjections of biologic agents may be the fastest growing area of orthopaedics and sports medicine. Cortisone is out, and anabolic therapy (stimulating tissues) is in. Here is a brief summary of our choices today—with the understanding that we are actively engaged in research to improve and target these injections for the future.
The broad field of anabolic injections focuses on stimulating injured tissues to heal—accelerating healing, shutting down inflammation, limiting scar formation, and recruiting the body’s stem-cell-derived self-repair cells. We no longer focus on injecting cells directly. Specifically, we do not inject bone marrow, fat-derived cells, or cells grown into a tissue culture. Since the body has billions of stem cells and their derivatives, and since directly injected cells die quickly, it makes more sense to recruit the body’s own vast reserves of healing agents.
We do this with proteins called cytokines. Cytokines and growth factors are chemical agents: the products of the cells that direct the entire symphony of healing. In a double-blind trial of biologic injections, we were able to identify the biochemical changes occurring within arthritic knees in the first week after injection and track the improvements in patients— improvements that lasted up to one year after a single injection.
Since an arthritic knee is different from an ACL-injured knee or a knee afflicted with tendonitis, the future will bring customized injections that produce more targeted responses. Meanwhile—as we await the results of further studies—we combine PRP with HA to create a broadly stimulating "cocktail." Here are descriptions of each ingredient.
Platelet-Rich-Plasma (PRP)
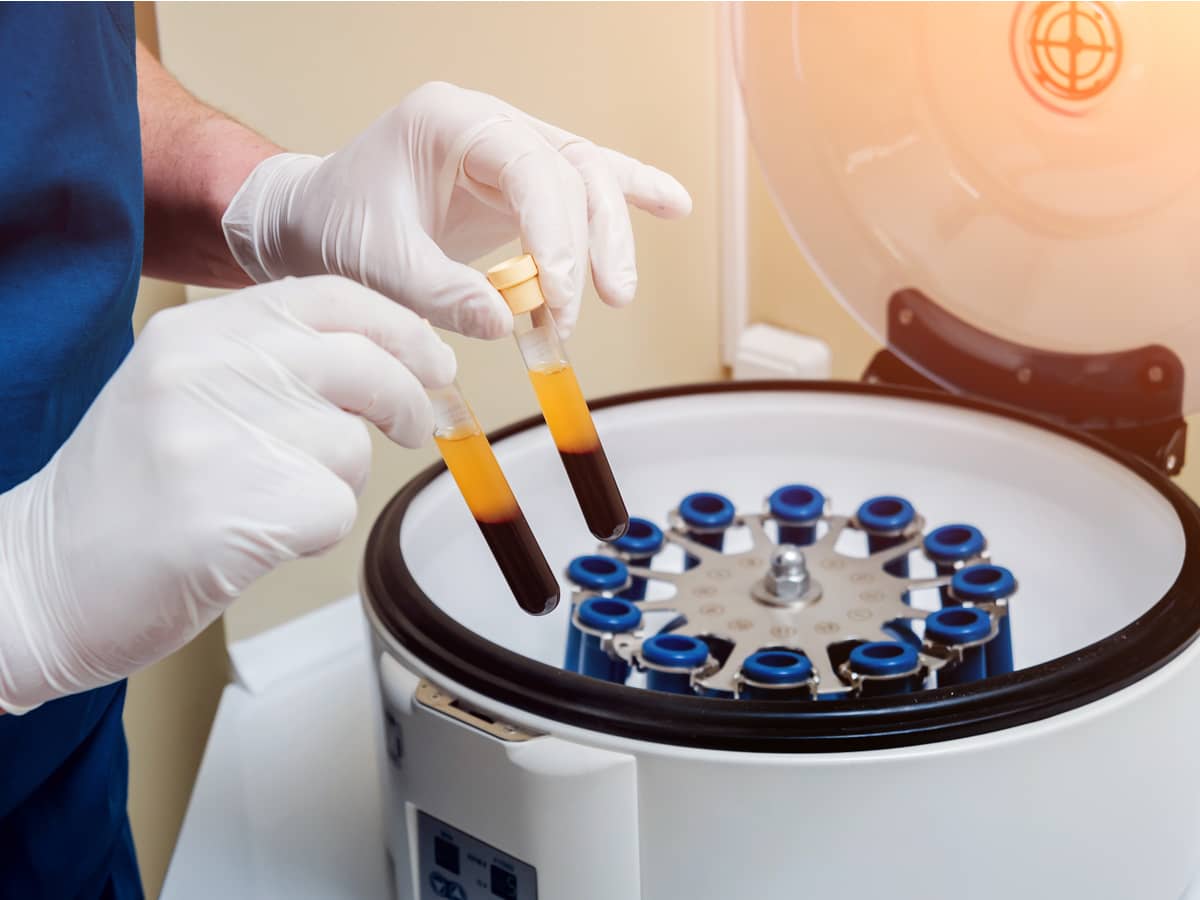
PRP (platelet-rich-plasma) is obtained by concentrating a patient’s own blood platelets, then injecting them into the site of injury.
Why we use PRP
The platelets have high concentrations of growth factors and cytokines. These stimulate tissue healing, reduce inflammation, and recruit the body’s own stem-cell-derived self-repair cells. The positive is that PRP comes directly from you, the patient. The negative is that PRP platelet and growth factor concentration varies in each person, even by the time of day. Therefore we inject a double dose of PRP when we are treating joint problems and almost always in combination with a double dose of hyaluronic acid.
What to expect
When combined with other factors (HA) we see relief of pain and inflammation generally peaking at one month and lasting up to one year in arthritic joints and damaged tissues.
Hyaluronic Acid (HA)
HA is the natural lubricant of all joints. When injected, it lubricates the joint surfaces, decreasing pain.
Why we use HA
HA is more than a great lubricant—it also acts as a carrier, dispersing injections of growth factors and cytokines around the tissues. When used alone, the beneficial effects of HA included great relief for some arthritic patients, though this usually declined after a short time. Our research study showed, however, that when HA is used in combination with anabolic stimulants (growth factors) the cells of the joints produce more lubricant and the benefit lasts longer.
What to expect
When the injections are combined, the body responds by decreasing inflammation and increasing cell turnover, lubrication, and repair. Pain is relieved over the course of one month and lasts up to one year.
But no injection alone is ever enough. Injuries and arthritis are opportunities to focus on becoming fitter, faster, and stronger than you have been in years. We combine every injection with rehabilitation. Our team will work with you to create a fitness program designed to help you become better than you were before you were injured.
The Future
Over time, anabolic injections will become more specific to each injury. By combining knowledge of the patient’s injury and their DNA-elucidated proclivity to respond to one factor or another, the injections will stimulate the correct physiologic response for each joint and tissue environment. Following significant clinical trials under the FDA, donor birth tissues will be sourced for their wide range of growth factors and cytokines useful for possible tissue regeneration. Eventually, with the right stimulation, tissues previously thought unable to regrow will respond with near-complete regeneration.
For some of these applications, though—especially in treating knee arthritis—the future is already upon us.

