Alternatives to Artificial Knee Replacement Reviewed
Hear From Our Patients
25-Year-Old's Disaster Knee Saved by BioKnee ProgramHere is a short review of the most common alternatives to knee replacement surgery.

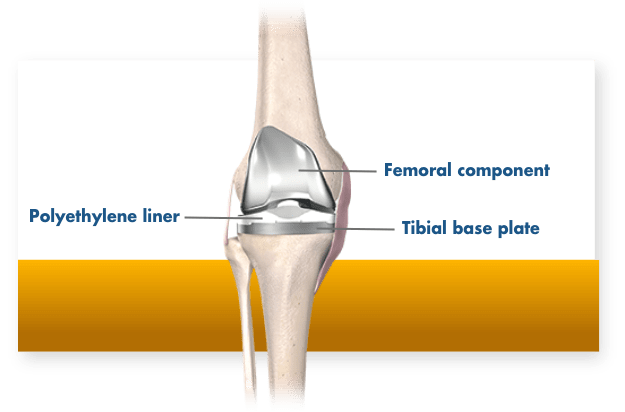
Artificial knee replacement surgery involves resurfacing the femur with a cobalt chrome metal cap and the tibia with a titanium tray, on top of which sits a replaceable polyethylene insert. Sometimes a button of polyethylene is also placed on the patella.
While this procedure works well for people with severe arthritis involving most of the knee joint, about 80% of people told they need a total knee replacement actually don’t. They could instead have one of the nonoperative treatments listed below, a biologic knee replacement where the meniscus and articular cartilage are replaced or regrown, or a partial knee replacement where only one part of the knee is resurfaced with metal and plastic. Here are some of the most popular alternatives:
Bracing
The pros and cons of wearing a brace for an arthritic knee are many. On the positive side, a brace can limit motion, apply pressure to one side of the knee in order to unload the pain side, or just provide warmth from compression. The cons are that braces are awkward to use, the benefits don’t last very long, and stiffness often occurs.
Walking Aids
Crutches, canes, and mobility devices unload joints. When forces like bearing weight are decreased, the joint surfaces become a little less stressed and often less painful. The cons are that these “aids” often limit activity, are clumsy to carry around, and really don’t solve the underlying problems
Physical Therapy
Arthritis leads to joint stiffness and loss of motion. The less range of motion in the joint, the more wear on a smaller area, leading to faster degradation. Physical therapy, when focusing on manual hands-on therapy, is a godsend for many arthritis patients. It mobilizes the tissues, increases the range of motion more than you can do on your own, and optimizes a strengthening program. The cons are the cost (though insurance will often cover a limited number of visits) and the hassle factor in getting to a therapist’s office. Online or virtual therapy can be helpful, but it is nowhere near as good as a great manual therapist.
Cortisone Injections
Corticosteroids shut down cell metabolism, therefore decreasing the fluid produced inside joints and the pain associated with it. The problem is that steroids also weaken tissues (less cell metabolism equals less collagen production) and lead to higher rates of infection.
PRP (Platelet-Rich Plasma) Injections
PRP is a concentrate of the platelets from the bloodstream. Platelets contain granules loaded with growth factors and chemokines that reduce joint swelling, stimulate cellular activity, are antifibrotic, anti-inflammatory, and antibiotic and immune modulating. They also recruit the body’s own reservoir of stem cells to the site of injury. Other than cost, there appears to be no downside. When combined with a lubricating fluid such as hyaluronic acid, pain relief can be extended to 18 months in many instances. The one problem is that it doesn’t work for everybody and eventually becomes less effective at reducing the pain of arthritis.
Arthroscopic Surgery/Debridement
All arthroscopic surgery is not the same. The cleaning out of torn tissues, loose bodies, and bone spurs from an arthritic knee has been incredibly helpful for many of our patients, specifically when the tissues are causing mechanical problems such as catching, locking, limiting motion, and swelling in the joint. Unfortunately, studies that focus on just one part of the arthroscopic procedure often fail to show definitive relief. Insurance companies often use this generic study data to limit reimbursement. But that view is not held by many top surgeons, who choose which patients can benefit and which steps to take in the surgery. Arthroscopic surgery in which tissues are regrown or replaced is very different from just debridement alone.
Osteotomy
Changing the alignment of the bones in an effort to optimize the mechanical forces in the joint can help delay the progression of arthritis and improve the symptoms. Unfortunately, the complication rates from osteotomies are high, the good outcomes are measured in years and not decades, and the damage to future artificial joint replacement results is real. Few patients return to high-level sports after osteotomies.
Microfracture
Though this procedure has demonstrated benefits for athletes in the short term, the results have generally not lasted. In its place, we perform an articular cartilage paste graft procedure, while other surgeons use procedures such as MACI, OATS, and cartilage stimulation procedures for isolated cartilage lesions. Though they can add years of relief to damaged joints, only paste grafting has been reported to work well in arthritic lesions.
Biologic Knee Replacement (BioKnee®)
In the hands of surgeons with expertise in replacing meniscus cartilage, regrowing damaged articular cartilage, and restoring ligaments in arthritic knees, the results of biologic knee replacement for arthritic knees have been gratifying, with long-term delays in coming to total joint replacement surgery. The Stone Research Foundation published our data on patients over 50 years old, referred for partial or total knee replacements, who chose a biologic replacement. Over 40% of patients delayed their need for an artificial replacement for 8 years, and the other patients never came to a partial or total knee replacement in the course of a 2-25 year outcome study1. The cons of this approach are cost, longer rehabilitation times, and reinjury of the biologic tissues.
Partial Knee Replacement
The introduction of robots to surgery two decades ago dramatically improved the precision with which metal and plastic implants can be placed into the knee joint (and now the shoulder, hip, and spine). This permitted a wider group of surgeons to develop partial knee replacement expertise, and for total knee replacement surgeons to more frequently abandon the use of bone cement. (The precise robotic cuts allow porous implants to be placed perfectly against the bones, allowing the bone to grow into the implant.) Partial replacement results in a faster recovery, a return to full sports, and preserves the option for resurfacing the rest of the joint at a later date if necessary. Partial knee replacements feel much more natural to patients than full replacements.
The range of options for patients continues to expand. The goals of treatment include pain relief, range of motion improvement, and return to active lifestyles. Our general guideline is that if there is still joint space visible on X-rays, alternatives to metal and plastic are viable. Once the joint collapses to bone-on-bone, the success rates of the non-operative options and biologic replacement options decline. That said, I have many patients with horrible-looking X-rays with no joint space who come in every Fall and say “Doc, I am not letting you operate on my knee until those cocktail injections you give me stop working…They get me through the ski season, and that’s all I need.”
I can’t figure out in advance which patients those injections will work for, and if I am doing good or just helping my patients further destroy their joints. Either way, their smile lights up our lives.
Citation
- Stone, K. R., Walgenbach, A. W., Slatter, S., Turek, T. J., Ferguson-Dryden, C., Dicker, M., Miltenberger, E., Cowles, H., Liu, V., Wu, S., & Vessal, M. (2024). Meniscus allograft transplantation in conjunction with arthroscopic biologic knee restoration delays arthroplasty in patients older than 50 years. Arthroscopy. Advanced online publication. https://www.sciencedirect.com/science/article/pii/S0749806324004183?dgcid=author


