What's New in the Disc
To the public, the science of back disease seems stuck in the days of often ineffective choices: tolerating the pain, taking medications, physical therapy, injections of cortisone, surgical disc removal, or fusion. To scientists, however, the spine is a hot area of research and new therapies. Here is one, focusing on the disc.
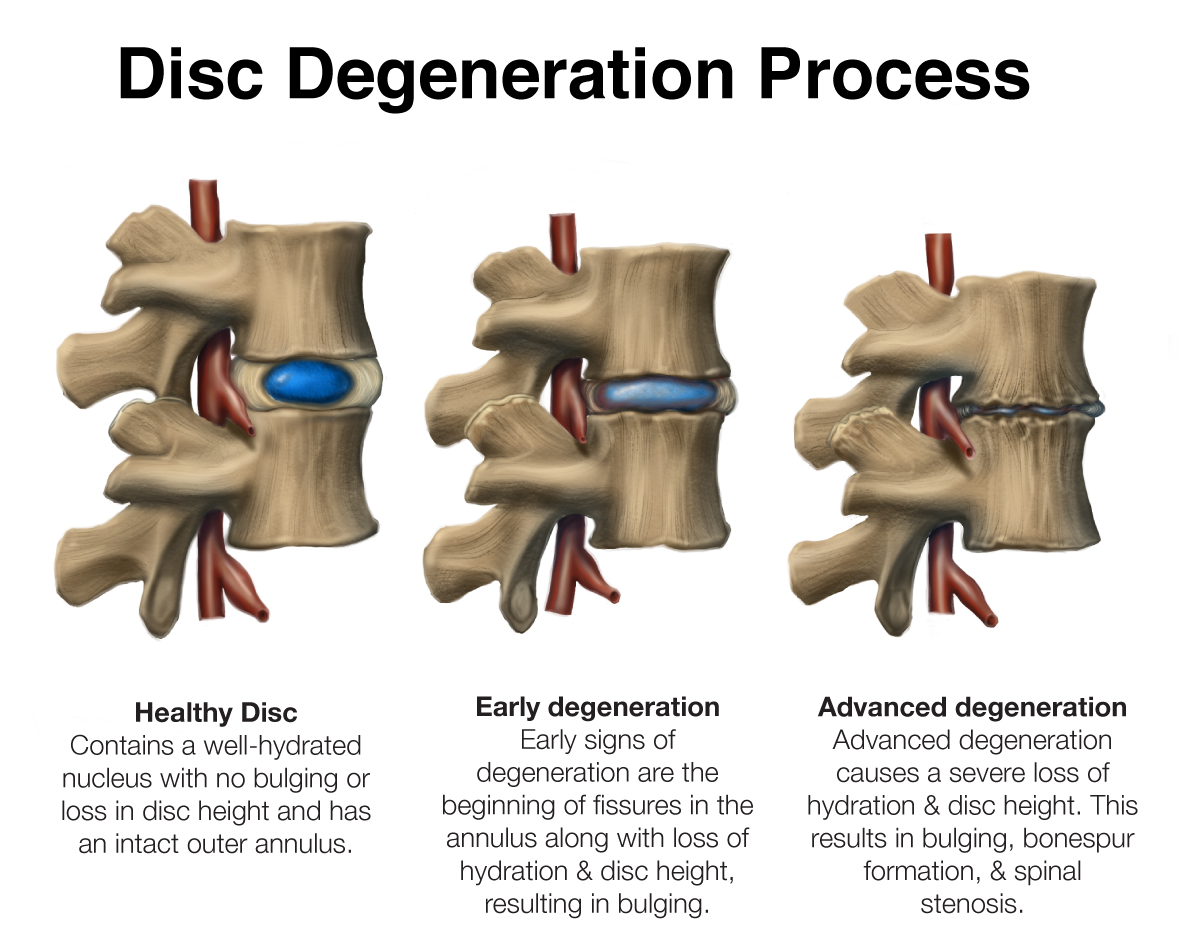
Original artwork by: Katerina Salsman
The intervertebral disc of the spine is made of a gelatinous material, surrounded by a ring of fibrous tissue called the annulus. Injuries to the annulus can cause the tearing of these fibers. This can lead to a loss of containment of the gelatinous material, and the biomechanical function of protecting the spinal column. Small tears in the ring are known to heal on their own, while larger tears lead to disc extrusion. When a disc pushes out of its annular ring, compression of the local spinal nerves leads to pain and loss of muscle strength.
The pain is often treated with the series of therapies noted above. If medicines and physical therapies fail, a more invasive approach is taken. Cortisone injections shut down cellular metabolism, reduce inflammation, and provide temporary pain relief. They are, however, associated with cell death. What’s more, they increase the rate of infection and provide no stimulus for healing of the damaged tissues
Ultimately, a surgeon may remove the protruding part of the disc. But there is a relatively high recurrence rate—due to the surgical approach itself or failure of the annulus to heal. Fusion of the opposing vertebral bodies is an option that does relieve the pain however limits spinal motion and leads to arthritis above and below the area that was fused.
What is new in spinal care is the identification of the cells involved in annulus regeneration—first in the neonatal cells of mice and now in adult humans. These progenitor cells proliferate and differentiate into collagen expressing anulocytes (cells specific to the annulus). Novel therapies, including injections of growth factors from platelets and other sources, are now being deployed to stimulate a healing process in patients who present with an injured annulus and disc disease.
The degeneration of the intervertebral disc is itself a stimulus for further disc disease progression. What this means is that, as disc degeneration begins, the normal cells of the disc are affected by the harmful enzymes released by the dying cells. Removing these dying cells with novel injection compounds and changing the environment from catabolic (degradative) to anabolic, appears to promote both disc healing and regeneration.
The complex role of inflammation at the disc level is just becoming understood; it’s both a positive and a negative. The initial inflammation from an injury recruits the body’s own stem cell (or progenitor cell) derived self-repair cells. This is a critical step in the healing process. Chronic inflammation, though, leads to a breakdown of the collagen tissue and degeneration of the structures.
Thus, there may be a strong reason to step in—relatively early in the healing process—with injections of growth factors. These factors stimulate the body’s repair process, just after the initial inflammation, by helping to augment stem cell recruitment and prevent disc degeneration from occurring. The old days of “wait and see what happens” will likely give way to early intervention with anabolic injections, during the “Goldilocks” window a few days or weeks after the injury.
Prevention remains the key to back injuries, with exercise programs that focus on flexibility, strong abdominal muscles, and weight optimization. Treatment of spine injuries, when they occur, will now focus on repair, regeneration, and restoration of normal anatomy. And what a relief that could be, for the millions of people who suffer from back pain and disease.
References:
- Torre OM et al: Neonatal annulus fibrosus regeneration occurs via recruitment and proliferation of Scleraxis-lineage cells. NPJ Regen Med. 2019 Dec 20:4:23
- Sloan SR et al: Combined nucleus pulposus augmentation and anulus fibrosus repair prevents acute intervertebral disc degeneration after discectomy. Sci Transl Med. 2020 Mar 11:12 (534):eaay2380
- Matsuda M et al: Recapitulating the human segmentation clock with pluripotent stem cells. Nature. 2020 Oct: 580(7801):124-9. Epub 2020 Apr 1
