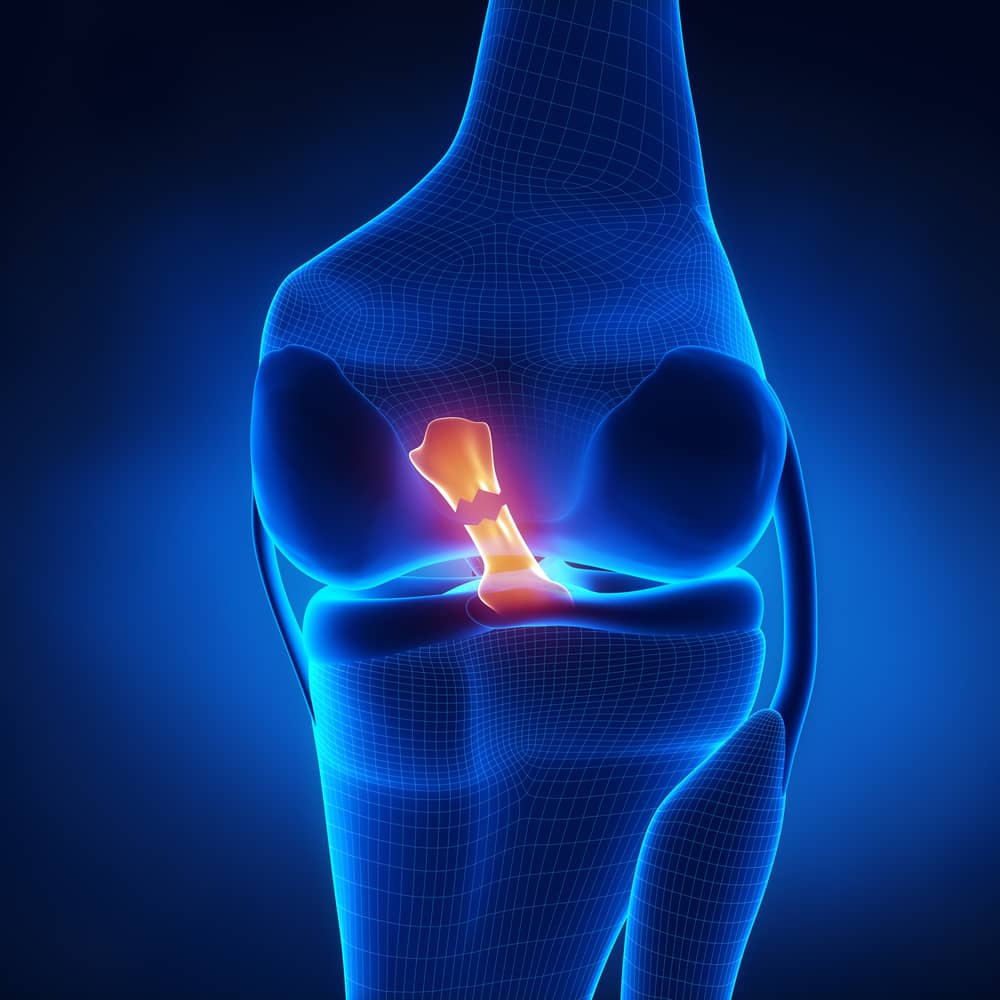
What is New in the ACL
The anterior cruciate ligament (ACL) continues to be the athlete’s Achilles’ heel. The ligament, once ruptured, leads to knee instability and, eventually, arthritis. The reconstructions return most people to sports—but not without a 50% incidence of arthritis after 10 years and a too-high failure rate. Unfortunately, reconstruction of the ACL is still not performed by surgeons with accuracy or consistency, and long rehabilitation times are required, so there is a renewed push to focus on primary repair of the torn ligamentous fibers. So what is new in this equation?
The old is new, again. ACL repair rather than replacement (commonly called reconstruction), first pioneered in the 1800s, is being reevaluated. The story of ACL repair improvements is as old as the surgical treatment itself, with every new generation of surgeons and scientists trying to identify which patients will do well with a repair, which new techniques work, and which biological or artificial additives can help improve the outcomes.
Sorting out which injuries will do well with a repair, which do well without surgery, and which require reconstruction is still not clear.
Here are today’s highlights.
Collagen scaffolds are being added to the top of the ligament, in hopes that the healing of the ruptured ACL to the bone will be more effective than suture repair alone. This effort, recently approved by the FDA, is likely to succeed in ligaments with little damage, and certain isolated injuries. But it will prove inappropriate, or fail, in injuries where the entire structure of the ligament is damaged. And most often the entire ligament is involved.
Growth factors from PRP, bone marrow, fat, and birth tissues are being added to most tissue injuries and surgical repairs. It takes a full year for an ACL reconstruction to remodel into a strong replacement. Growth factors may be able to speed this process by recruiting the body’s own progenitor and self-repair cells to the injury. Today we always add these bioactive factors to every donor graft we use.
Permanent reinforcements—such as internal braces made of suture materials—are also in vogue. These devices have the benefit of being easy to insert. While they provide immediate stability, they stress-shield the healing ACL fibers—often leading to scar formation rather than true ligament formation.
True artificial replacements of the ligament from multiple materials—including carbon fiber, Gore-Tex, polyethylene, and others—have been shunned in the US due to their high failure rates. In some countries, however, these grafts have continued to be used in certain situations with success. New constructs will be tested again in the US, with the benefit of decades of data on which patients are right for artificial replacement ligaments.
Xenograft ligaments were successfully tested in the US in a pilot trial and have performed as well as allografts in a wide clinical trial in Europe and South Africa. Unfortunately, the entire study was confounded by an avoidable manufacturing error, which permitted a water-borne infectious agent to slip into the final processing. Investors closed the company. But this promising technology will come back, as the successful patients in the first clinical trial are still successful almost 20 years later.
Prevention remains the best option. ACL injury prevention programs work when athletes start early. This is especially true for women, who have a 5-8 times increased ACL rupture rate.
ACL vaccines are not yet envisioned; but as we learn how to use mRNA technology to induce muscles to produce specific foreign proteins, we may one day be able to inject the unique ligament cells to produce specific, aligned, stronger collagen—thereby preventing some injuries entirely and enabling a stronger repair in others.
In the case of ACL vaccinations, the new will be really new.

