Revision Cartilage Repair
Articular cartilage covers the ends of bones in all human joints. Techniques for repairing damaged and arthritic bone surfaces are improving. Here are the highlights of the science and how to rescue joints when initial intervention fails.
Articular cartilage, when injured, heals poorly—if at all. The shiny white surface has a natural lubricant called hyaluronic acid, which permits joints to move with a slickness of five times that of ice on ice. It is a magical surface—until injured by trauma or damaged by disease. Articular cartilage lacks a blood supply. Its cells are widely spaced with an extracellular matrix made up of water and charged sugars (called proteoglycans) that attract the water and release it when compressed. Even without trauma or disease, this sponge-like mechanism tends to become more brittle with age as the balance of these charged sugars shifts to a less pliant combination.
Injuries to the knee joint ligaments, such as the ACL, lead to instability in the knee. The resulting abnormal motions cause excess wear, as with a tire that wears out rapidly when the car is out of alignment. Loss of the knee joint meniscus cartilage concentrates forces in the knee joint, accelerating the wear of the cartilage. Impact injuries like bone fractures can also damage the bearing surface.
In the past, it was believed that the articular cartilage could be neither repaired nor regenerated. This turned out to be false. Our clinic and others have tested cartilage repair techniques that have now lasted more than thirty years in our knee and ankle patients.
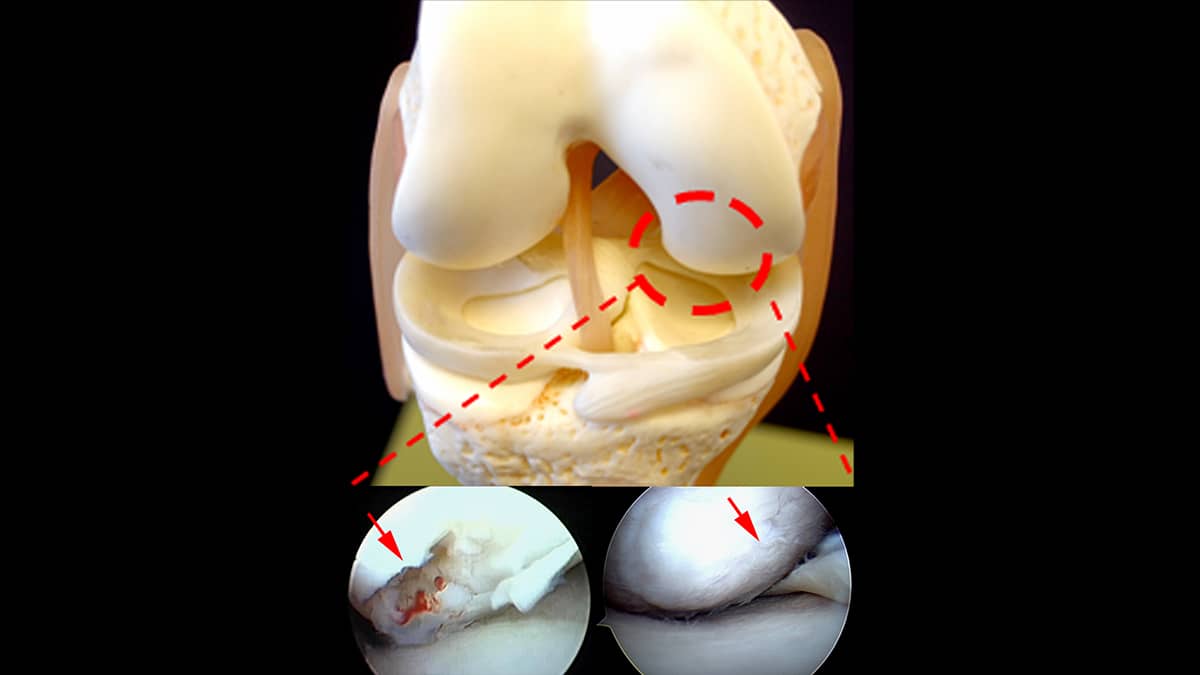
The first insight we made was that the cartilage in the intercondylar notch of the knee joint (where the ACL passes) regenerates relatively quickly after a notch-widening procedure that is often performed during ACL surgery. Secondly, we realized that the larger the injury, the more robust the healing response. In 1991, we began treating dead and arthritic areas of articular cartilage with a super microfracturing (aka morselization) technique, which releases the patient’s own bone-derived stem cells. When we applied a paste of bone and articular cartilage to the prepared lesion, new articular cartilage grew in beautifully. This healing response is similar to what we see in bone spurs, which are also covered in robust new articular cartilage.
This articular cartilage paste graft technique has worked well for us in treating primary cartilage lesions as well as arthritic surfaces—providing there is still remaining joint space. Other strategies have evolved recently as well, including a MACI technique (in which a collagen cover is placed over a cartilage lesion) and an OATS procedure (where a plug is impacted into a defect).
Overview of the Articular Cartilage Paste Graft Technique
The good news is that, most of the time, these procedures work—and even if they fail, paste grafting can be used to salvage them. For the weight-bearing surfaces in the knee, it is also important that the ligaments be stabilized, and the meniscus—if it is missing at the time of cartilage repair—be replaced. This entire effort, which includes replacing and re-growing the key tissues in the knee, is called a biologic knee replacement, or “BioKnee.”
Also improving is our ability to accelerate the healing of all tissues. This is achieved by the injection of growth factors and cytokines to the injured structures. These factors appear to work by recruiting the body’s native stem-cell-derived self-repair cells and by increasing lubrication in the joints. Our research is focusing on identifying the most potent of these growth factors and targeting them to specific tissues. This combination of tissue regeneration, tissue replacement, and anabolic stimulation of the healing process is revolutionizing our approach to healing damaged joints. Who would have imagined that working with nature’s own recipes could surpass the traditional metal and plastic joint replacements?

