Myths and Facts About Stem Cell Therapies
Hear From Our Patients
Non-Surgical Knee Pain Relief with Injections of PRP & HAStem cell therapies are growing in popularity—and rightly so, in my opinion. They are one of our greatest tools when it comes to stimulating damaged tissues within the body to heal. The importance of this cannot be overstated, especially when you consider that traditional therapies (cortisone, NSAIDs) often focus on suppressing the body’s ability to heal.
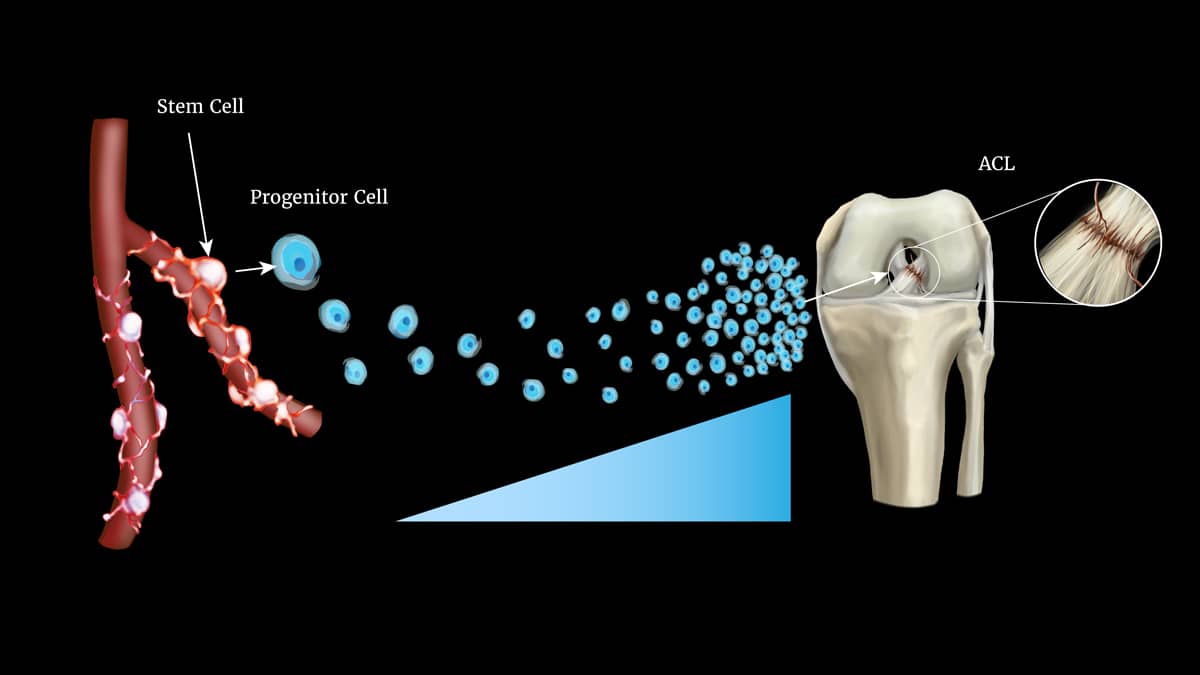
Illustration by Katerina Salsman
I have seen, in my own practice, how effective stem cell activation therapies are at helping people overcome injuries and arthritis. Patients often get incredible results from these therapies. In many instances, when combined with great fitness and rehabilitation programs, they can come back fitter, faster, and stronger than they were before they got injured or arthritis set in.
However, there is still a lot of misinformation around stem cell therapy. Many people don’t know, for instance, that we all have billions of stem cells within us. They don’t know what makes stem cells so beneficial or how we can use them to augment the healing response.
To take full advantage of these therapies, it helps to be able to sort fact from fiction. Here is an overview of what stem cells are, followed by a look at the top three facts and myths about stem cell therapy.
An Overview of Stem Cells
Stem cells are believed to be the precursor cell of all cell types. This means that they can transform into the specific cell type of the tissue they are trying to repair.
Stem cells predominantly live on the walls of blood vessels. There are also specialized stem cells that live within tissues, such as articular cartilage. The more blood vessels, the more cells.
At the time of an injury to a joint, or an insult to the body (such as a ligament tear), these cells are called into action. As local cells respond to local trauma, they send signals which recruit the army of stem cells lying in wait on the walls of blood vessels throughout the body.
These stem cells, when activated, divide and send a “daughter” progenitor cell to the site of injury. Those progenitor cells release growth factors, antibiotics, and other proteins and factors necessary for repair. The progenitor cells are so powerful that, together with the normal immune system cells, the chemicals they release kill most invading bacteria long before the host feels a reaction.
Three Important Facts About Stem Cells
First, everyone has billions of stem cells within their bodies. Though you do have fewer stem cells as you get older, you still have billions regardless of your age.
Second, the stem cells in your body are self-renewing. This means they can be induced to divide and release “daughter” cells, one of which replicates itself. They do this from their site of residence; in other words, wherever the original stem cell is.
Essentially, the stem cell divides, creating one copy of itself and one daughter (or progenitor) cell—which, unlike the stem cells it came from, is not self-renewing. The progenitor then migrates to the site of the injury or the disease. From there, it augments the healing response by directing other cells to participate.
Finally—and this fact is especially important to understand if you’re trying to figure out what stem cell therapy will be most effective for you—it is far more potent to induce your own cells to go to the site of injury than it is to inject external stem cells. How can you induce cells to go to the injury? By injecting chemotactic factors (for example, cytokines and growth factors) instead of injecting lab-cultured or aspirated stem cells.
Today, the most powerful recruitment factors in our clinic come from the proteins found in PRP (platelet-rich plasma), the concentrated platelets from a patient’s bloodstream. Injections of proteins from these platelets demonstrate anti-scarring, antibiotic, anti-inflammatory, and pro-stimulation characteristics. Arthritic patients’ joints produce more lubrication after injection and have less stiffness. Soft tissue injuries heal faster. This happens not just from the compounds in the injections, but from the recruited progenitor daughter cells that direct and release factors which induce healing.
Three Common Myths About Stem Cell Therapy
The first myth is that stem cells can regrow cartilage, ligaments, or organs. This is false—it is not how stem cells work. Stem cells divide to form progenitor cells. Those progenitor cells can turn into cells with a specific function: blood cells, bone cells, and so on.
The second myth you should watch out for, especially if you’re looking into stem cell therapy for yourself or a loved one, is that stem cells drawn from the patient’s bone marrow or fat and injected are as effective as local (endogenous) stem cells that have been induced to migrate to the site of injury. Again, this is not true: It is always more effective to induce endogenous cells to migrate than to inject bone or fat stem cells. The reason is that these cells are relatively low in number, often die soon after injection, and are not necessarily the correct cells for a specific problem.
The third and final myth is that stem cells can be grown outside the body and reinjected effectively. Stem cells that grow outside the body differentiate; this means they divide into daughter cells that are often influenced by the lab in which they are cultured. And the more often they divide, the less they are like the original stem cells. That means they are less effective at directing healing—which is the reason to use them in the first place.
Rather than stem cell injections, we are better off optimizing anabolic injections: a combination of cells, growth factors, and recruitment proteins (cytokines). These stimulate the healing response and, most importantly, stimulate the body’s own native stem-derived progenitor cells to migrate to the site of injury.
What This Means for You
Understanding these facts and myths is helpful, especially if you are injured or suffering from arthritis. Administered properly, anabolic injections are quite powerful when it comes to relieving pain.
For arthritic joints, injecting growth factors in combination with hyaluronic acid boosts the production of the natural lubricants of the joint. This makes the benefit from the hyaluronic acid injection last longer, providing pain relief often equal to that offered by anti-inflammatory drugs.
For soft tissue injuries, torn ligaments, muscle strains, and tendonitis, injections of anabolic factors accelerate healing by reducing swelling and scar tissue formation while simultaneously increasing new collagen production.
The bottom line: Anabolic injections and recruitment of stem cells are powerful forms of therapy that can spell relief for anyone suffering with pain from injuries or arthritis. You already have billions of stem cells within you. All we need to do is activate them and recruit them to the site of injury.


