Knees That Have Gone to Hell
Hear From Our Patients
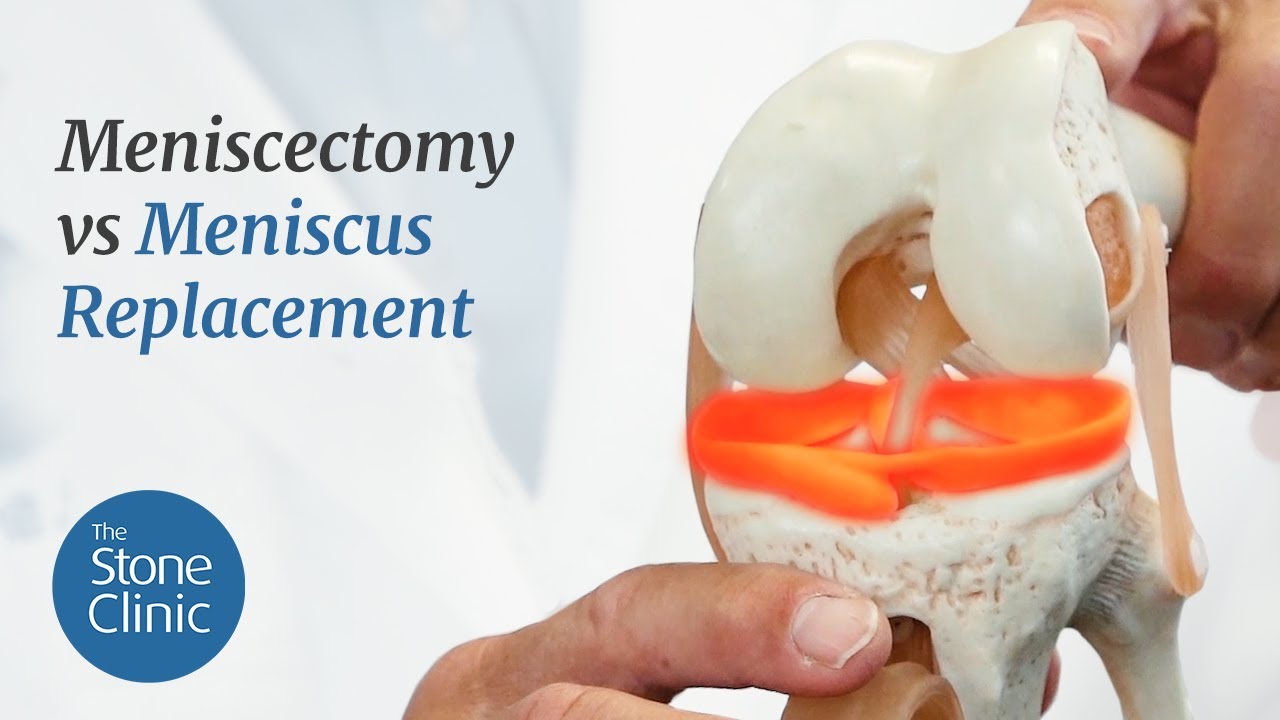
25-Year-Old's Disaster Knee Saved by BioKnee ProgramAfter a simple meniscectomy, most knees do well for a while. But some knees crash and develop significant pain and arthritis within six months. We call these “knees that have gone to hell.” Here is why.

The meniscus is the key shock absorber and protector of the joint articular cartilage. When even a small portion of it is removed, the force concentration on the top of the tibia is concentrated in a smaller area, leading to a higher level of wear. Usually, it takes years for the wear on the articular cartilage to develop into full-blown arthritis. Sometimes, however, for unknown reasons, certain knees decline very rapidly. By six months, there is the appearance of osteonecrosis— death of the bone in the side of the knee—where the meniscus was resected. This most commonly happens with women between the ages of 40 to 66, though it can occur in men and in other age groups as well. The process used to be called SPONK, or spontaneous osteonecrosis. Today, since bone death is not always present (but arthritis is) we simply call them “knees that have gone to hell.”
If the damage is not too severe, a biologic reconstruction of the knee—with replacement of the meniscus and regrowth of the articular cartilage using a paste graft technique—can be used to restore knee function. This procedure requires a significant dedication to a complex outpatient surgery, followed by non-weight bearing for a month, and a careful rehabilitation program for an additional four months. When done correctly, patients can return to full sports (impact sports are best delayed, optimally for a year, as the collagen in the meniscus and the articular cartilage matures.)
If the damage is severe, with loss of joint space, a partial knee replacement is the key to a pain-free return to sports. This is done as an outpatient procedure, under robotic guidance. Fortunately, by three months after the partial replacement, most patients have a “forgotten knee.”
The real key is to prevent the development of joint collapse in the first place by restoring rather than removing critical tissues. The knee joint is intolerant of loss of the meniscus cartilage and demonstrates its anger either very early (as in these hell-bound knees) or over time—as with the arthritis that develops, over decades, in knees that have undergone a meniscectomy. The solution is to repair all repairable meniscus tears and replace the tissue as soon as resection is performed. Though only a few segmental replacements have been done so far, we have found that, most of the time, if a significant portion of the meniscus is lost, it is best to replace all of it with a donor tissue.
Our segmental collagen scaffold for re-growing the defects (called the CMI) is no longer being offered by orthopaedic companies. We are working on a better version. So for now, if the meniscus is significantly damaged, repair it or replace it—or risk a confrontation between the devil and your knees.