What is a Partial Knee Replacement?
Hear From Our Patients
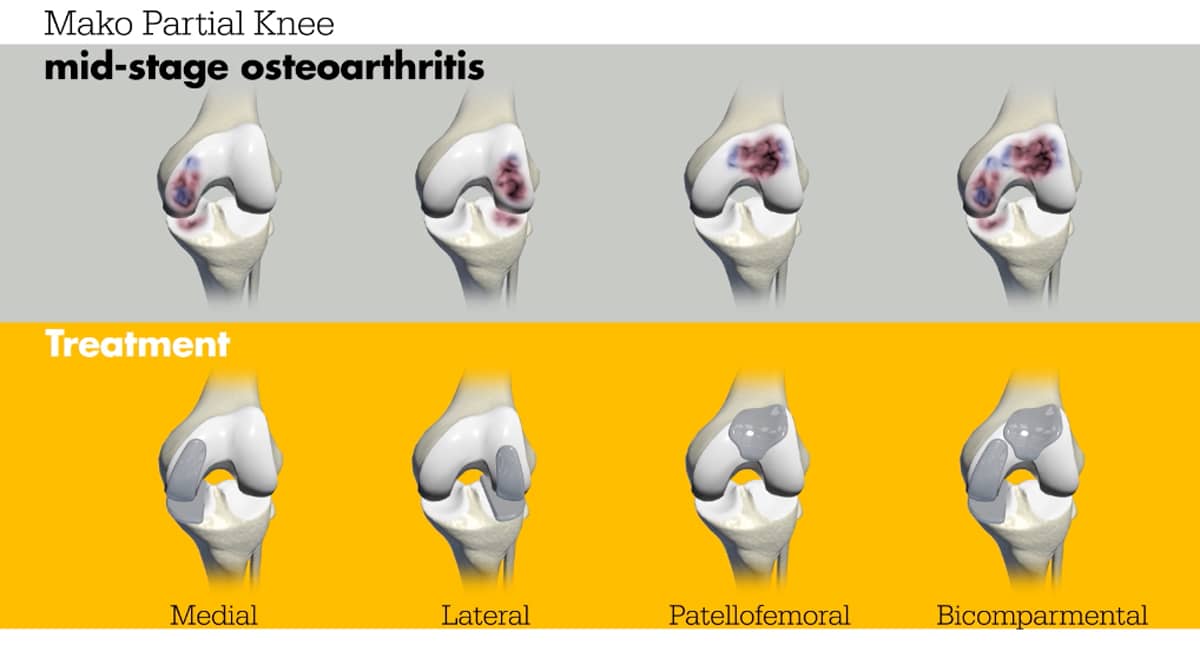
Partial Knee Replacement for Experienced Ultra Runner (3 Months Post-Op)The knee is generally divided into three components: the medial, the lateral, and the patellofemoral. The medial is the inside of the knee, the lateral is by the fibula (the long, thin bone in the lower leg, parallel to the tibia), and the patellofemoral around the kneecap. Most arthritis cases involve one or two of these compartments.

Understanding Partial Knee Replacement Surgery
Metal implants made of cobalt chrome are available to cover the individual ends of the femur (thigh bone). Titanium plates are used to cover the top of one side of the tibia. High molecular-weight polyethylene buttons are used to cover the patella and to act as an interface between the femur and tibia (like a meniscus). By resurfacing just the worn-out part, the remainder of the knee—including the ligaments—is left untouched.
Knees with partial replacements feel more normal than those that require full replacements. This is because the geometry of the knee remains intact and the ligaments naturally guide the knee. One reasonable analogy is that if you have a diseased tooth, you want only that single tooth capped—not a full set of dentures.
Advanced Imaging and Robotic Precision in Surgery
To perform a partial replacement using 21st-century surgical techniques, an X-ray, MRI, and CT scan are performed. Of all these imaging techniques, the X-ray best shows the bony alignment and joint space. The MRI shows the articular and meniscus cartilage as well as the health of the ligaments. We usually know that the worn-out part of the knee, presenting a bone-on-bone appearance on an X-ray, has no functional cartilage left. Still, we are curious about the health of the remaining compartments of the knee. If they are healthy, there is no need to replace them. If not, the question becomes: Do they need a soft tissue repair, a ligament replacement, or a multi-compartment resurfacing at the time of the partial replacement?
The CT scan is used to build a 3-D model of the knee. The metal and plastic components of the partial knee replacement are positioned on that virtual model. The ability to move the components to the optimal position in all planes, especially in rotation, is what makes computerized partial replacement far superior to the old hand-held methods.
At the outpatient surgery center, a robotic arm—programmed to follow the 3-D model of the knee—is guided by the surgeon. It removes only the area of damage and inserts the implants precisely. The surgery can be optimized by adjusting the thickness of the plastic insert, balancing the joint. This phase of the surgery, as well as all the fine adjustments of the implants and the handling of the soft tissues, is what differentiates top-quality surgeries and surgeons from average procedures and practitioners.
When to Consider a Patellofemoral or Bi-Compartmental Replacement
When the patella (kneecap) is worn down, it can be challenging to decide whether to perform a bi-compartmental replacement, a surgery that replaces either the medial or lateral compartment (the inner or outer half of the knee joint) and the patellofemoral joint (where the kneecap meets the thigh bone). Many patients do well without resurfacing the patella, as most of their pain comes from the medial or lateral side. Even in full knee replacements (replacement of all joint surfaces), we rarely resurface the patella. However, if the patella alone is worn down and X-rays show bone-on-bone contact (loss of cartilage), a patellofemoral replacement—replacing just the kneecap joint—can be the best solution.
Currently, all partial knee replacements are cemented in place, while most of our total joint replacements are press-fit and uncemented. The technology to make the undersurface of partial replacement implants porous—allowing bone to grow into them—has not yet received FDA approval. Hopefully, this will soon change.
How Activity After Partial Knee Replacement Protects Your Joint
Surgeon judgment, experience, and bias influence all these decisions. Many factors, including the bias of your surgeon, affect the outcome. Is he or she an athlete? Do their patients return to sports? Are they more interested in total knees than partial replacements? Are they comfortable with robotic assistance? We encourage our patients to return to full sports, because weight-bearing activity builds bone and strengthens muscles, protecting the joint over time. The old advice to “rest your knee” leads to osteoporosis, muscle atrophy, and eventual failure of the joint.
So if it ain’t broke, don’t fix it. If it is partially broken, fix only what needs to be fixed.
Hear From Our Partial Knee Replacement Patients Who've Returned to Sport
We have patients now running triathlons and (ultra)marathons, climbing mountains, skiing a hundred days a year, on the replaced parts inside their knees. Below is the story of one of our most ambitious athletes: ultra marathon runner Richard Donovan.



