Is Total Knee Replacement Right for Me?
A majority of patients who are told they need a knee replacement actually don't. What can a patient do to determine if they truly do need a knee replacement? In this interview, Dr. Stone discusses the main points that will inform the final decision made by patient and surgeon together.
What specific questions can a patient ask their provider during their office visit?
Dr. Stone: I think the real place to start is, what does the doctor ask the patient? This is where we narrow down the cause of the knee pain that’s bringing up the possibility of surgery in the first place. But even before we get into the pain, it is important to understand who the patient is. What are their goals and what activities and sports do they play (or want to play but can’t, due to the knee)? With this understanding, we then dive into the specifics of their presentation.
The next question is, where do you hurt? If the patient says, “I only really hurt on one side,” or “I hurt when I'm going up and down stairs,” that focuses the physician on where the problem is. And it turns out that about 80% of people who have been told they need a knee replacement, don't—because most people have serious damage on one part of the knee, and not on the other.
The second question is, when do you hurt? Do you hurt lying in bed? Do you hurt when you're walking? Do you hurt only when you jump, or when you're hiking up and down a mountain? These questions will help the surgeon focus on what the real problem is. Is it a torn meniscus? Is it instability of the knee, or is it arthritis? That’s why the next thing we ask is, how far can you walk before you have pain? And when does the pain kick in? That helps us differentiate quite a bit about the degree of arthritis.
Then we ask, what makes your knee feel better? Do you take medications, or ice it? Have you had any injections? What do you do that makes the pain go away? Because while inflammation pain usually responds to anti-inflammatories and icing, arthritis pain—the achy, deep pain people have with arthritis—doesn't always go away with those treatments.
The next part of the exam involves watching the patient walk. We learn a ton from watching how somebody walks. Do they walk with bow legs, versus with knock knees? Do they walk with a limp? Do they have muscle weakness? And do the rest of the joints that are attached to the knee work well, or does the patient have a floppy foot, tight hips, or other limitations? Also true from watching them run up and down the hallway in the clinic.
Finally, we do an actual physical exam, which gives us a host of information about whether or not someone really needs a knee replacement. As part of this, we look at range of motion. Where is the joint tender? Is there grinding or cracking? Is it isolated to one part of the knee or the other? The most obvious mistake a surgeon can make occurs when someone's complaining of knee pain—but on examination, we find that they have no hip motion. That’s because, very commonly, hip arthritis radiates to the knee. And woe be the surgeon who operates on the knee when the generator of pain was really the hip.
That brings us to the next question: What areas have to be irreparably damaged to merit a total knee replacement?
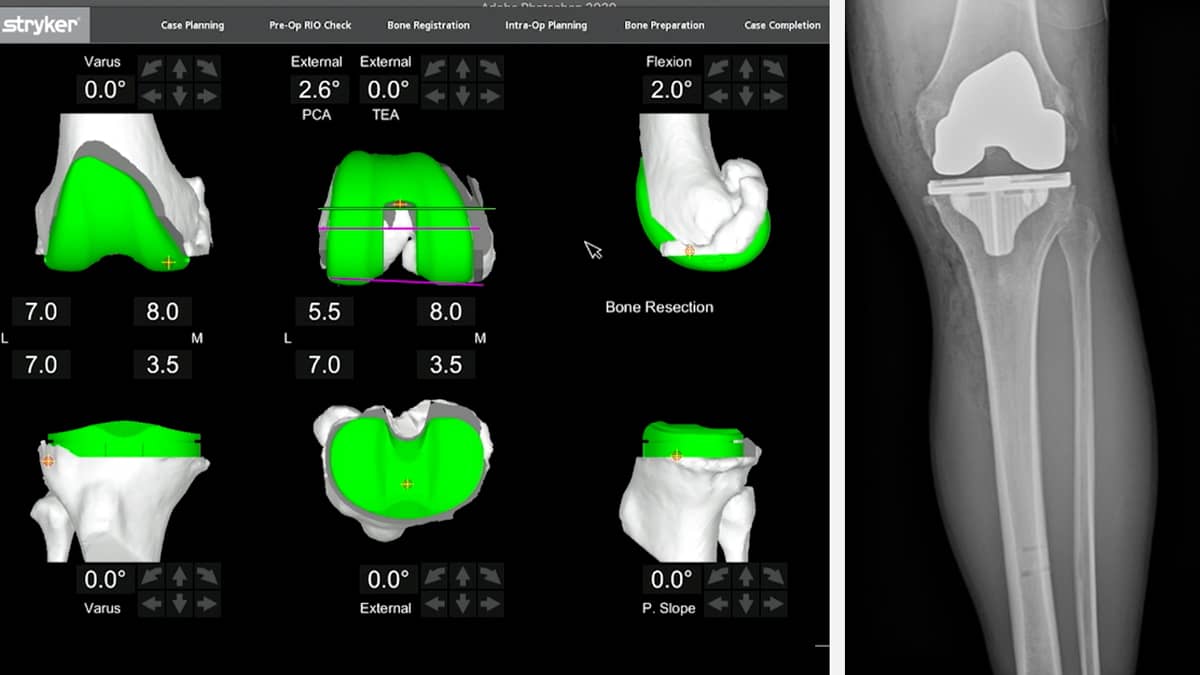
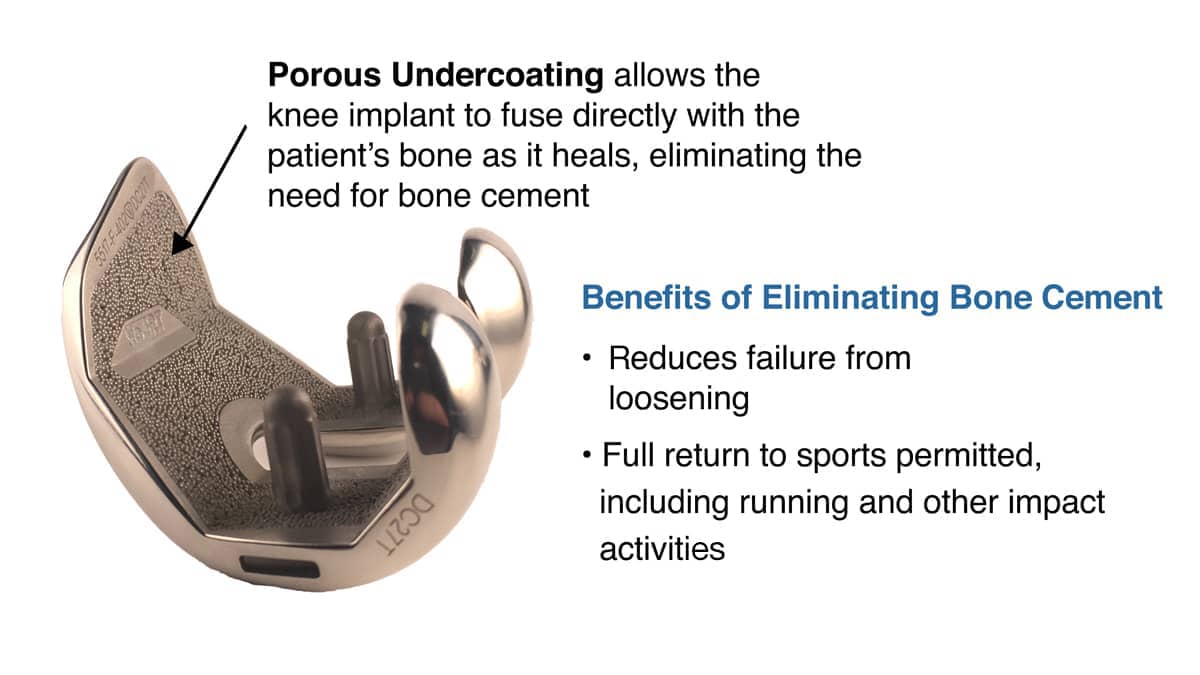
Dr. Stone: We only do total knee replacements when there are bone-on-bone changes in more than one part of the knee. And when we do, we use robotic control to maximize the precision and minimize the bone loss. This also permits us to use bony ingrowth components (metal pieces that the patient's bone grows into) so that the cement, commonly used to fix the implants, is eliminated. No cement means it is extremely unlikely to ever come loose, even with a return to full sports.
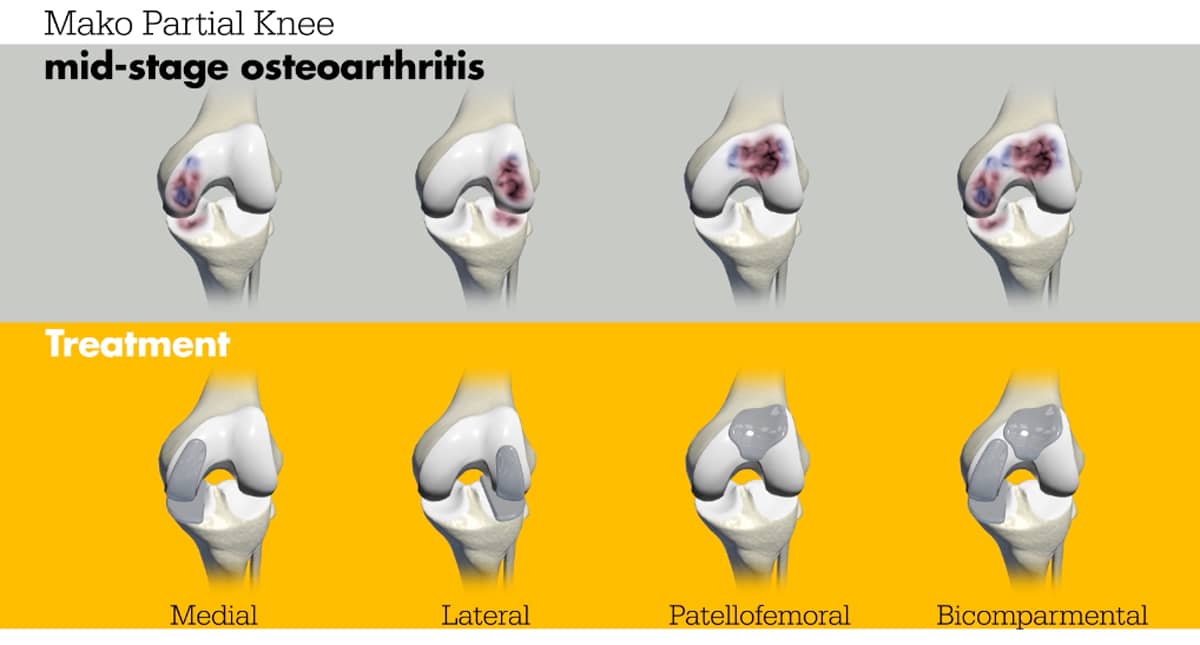
If there's a bone-on-bone change in just one part of the knee, we can either do a partial knee replacement—where we just resurface one part of it—or a bicompartmental, where we resurface two parts of the knee. Partial knees involve less surgery, feel more normal, and have faster recovery times back to full sports. 98% of patients say it is a forgotten knee between three and four months.
If there's arthritis, but no bone-on-bone changes, we may have an opportunity to do a biologic reconstruction, where we regrow the cartilage or replace the meniscus. And our biologic injections of growth factors and lubricants often help the patient buy time to consider their options.
At what point should a patient seek a second opinion about whether or not they need a replacement?
Dr. Stone: Whenever they're told they need a total knee replacement. Because you always need to know the bias of your surgeon. If the surgeon is biased towards doing total knee replacements, then every time they see arthritis the patient will be told they need a total knee replacement.
Whereas if the surgeon's bias is towards doing biologic reconstructions, they're often going to be offered those options. But if the surgeon isn't trained in either biologics or partials, the patient will never hear about it.
So, I believe that, whenever you're given a dramatic diagnosis or a dramatic solution without other options, it makes sense to look around a little bit to understand the other options. But if the surgeon explains the various options carefully, along with the pros and cons of each approach—and why they think one approach is better for one patient than another—then you, as a patient, may feel sufficiently well informed. But if the surgeon just takes a “one and done” approach, I think it's important for the patient to look around and think about it.
How does a patient learn what their surgeon's bias is?
Dr. Stone: Just ask 'em. It’s surprising, but patients frequently don't ask those questions of the surgeon. What is the surgeon most comfortable with? What do they do most frequently? What do they not do, and why? Is the surgeon using the latest robotic technology? Are they able to avoid using bone cement when fixing the knee implant? Do they let their patients exercise fully, or do they limit them, and why? Do they use immediate physical therapy? It's totally reasonable to ask these questions.
I guess many patients don't have enough self-confidence to feel that they can ask the right questions.
Dr. Stone: Well… if they have well enough confidence to have somebody operate on their knee, they ought to have enough confidence to ask a question about it before it gets cracked open.
Dr. Stone Explains Our Alternatives to Total Knee Replacement
Our BioKnee® program biologically reconstructs the knee joint without the use of artificial implants. Head here to learn about our alternative to knee replacement.