Failed ACL
Hear From Our Patients
ACL Surgery Revision Reconstruction Patient 6 Years Post-opThe goal of ACL surgery is to stabilize the knee joint, return it to normal mechanical function, and permit the athlete to resume sports without a deficit. This outcome is not always achieved. Here are the most common reasons I see failures and what can be done about it.
Commitment. To have a successful ACL surgery the patient, surgeon, and rehab team must be committed to a specialized program. This includes six elements: achievement of anatomical surgery with accurate restoration of all the injured tissues; dedication to an immediate rehabilitation program with the goal of obtaining full extension in the first week; soft tissue massage to remove the swelling that slows healing; a fitness program that starts immediately to strengthen the core, improve the cardiovascular capacity, while optimizing balance and coordination; a nutrition program that augments healing; and mental training program that promotes optimism, vision, and patience.
The failure of any one of these critical components leads to the failure of all of them. When a patient comes in with a “bad” knee after ACL surgery, investigating what went wrong with each or any of those six elements is the first step toward a successful outcome.
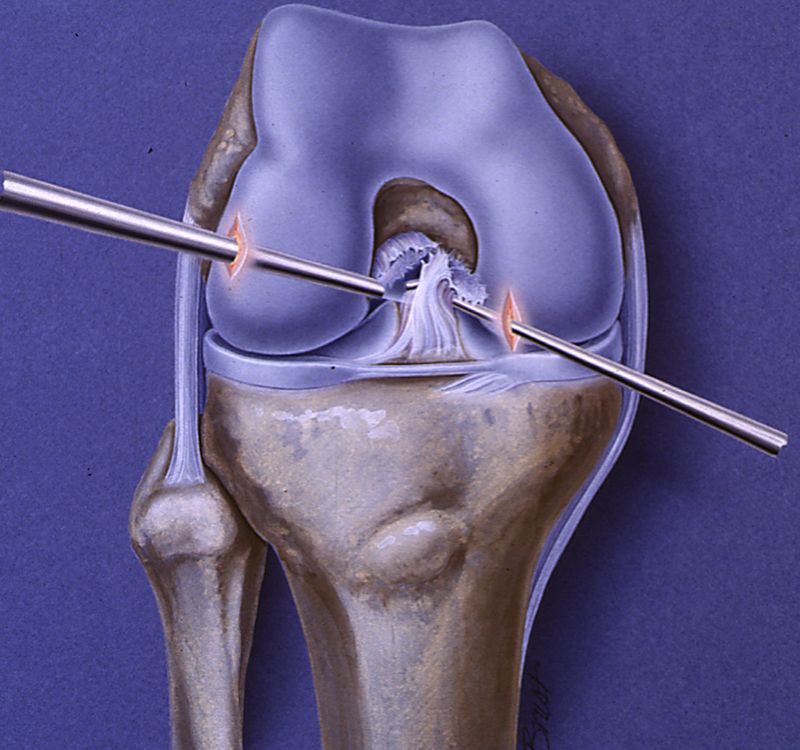
Surgery. The ACL is a strong ribbon of tissue that extends from a ridge on the femur to a curvilinear area on the tibia. When ruptured, the entire ribbon suffers from internal failure and must be replaced. The event that ruptures the ACL, however, often tears other tissues as well. Some, like the meniscus, are usually obvious. Others are more subtle—as with tearing of the corners of the knee joint, where only a thickening of tissue capsule provides crucial rotational support.
Too often the surgeon only reads the MRI report or examines only the ACL, ignoring subtle injuries to the other tissues that guide the knee. Unrepaired, these injuries force the ACL to support all the rotational forces of the knee, leading to a gradual stretching out and failure. The solutions are:
- Replace the ACL anatomically, exactly matching the natural insertion areas.
- Use strong replacement tissues, such as the patellar tendon. Our preference is to use donor patellar tendons, so as to not produce a secondary injury to the knee.
- Repair, not resect, damaged meniscus tissue. Once the meniscus is removed—even portions of it—the stabilizing effect that protects the ACL and the joint is diminished, leading to further ACL strain and joint arthritis.
- Repair and reconstruct the peripheral tissues (e.g., the posterolateral corner or the MCL) if they are injured. When we see failed ACL knee surgery, it’s often because the ACL is placed too high in the notch above the natural insertion site or too far anterior or too vertical. The meniscus is often missing and the rotational stability of the knee lacking. We replace the ACL, insert a new meniscus from a donor, and reconstruct the corners of the knee.
Rehabilitation. Even perfectly placed ACLs can fail due to poor rehabilitation. The most common presentation is a stiff knee with loss of full extension equal to the opposite side. Overwhelming data shows that if the knee does not extend equally to the opposite side, the knee will not feel normal—and the knee cap or patella will wear out, leading to anterior knee pain.
The second most common presentation is the weak, atrophied leg. Bioactive factors that are potent anti-inflammatories are offering hope for these stiff, failed ACL knees. Cortisone is never used, as it leads to cartilage damage and weakening of the tissues. The newer injections, combining PRP with Hyaluronic Acid lubrication, assist therapy and improve revision surgery outcomes
The ACL injury and surgery can often lead to ACL depression syndrome, where the patient becomes depressed due to the disruption in their lives from the unexpected injury, the surgery, and the pain they experience. Almost all patients have some degree of this let down three to four weeks after surgery. When the depression becomes severe—and is combined with a lack of supervised fitness training and physical therapy with hands-on soft tissue massage—a person can become a knee cripple. Reversing this is completely possible, but it takes dedication on all levels.
Failed ACL surgery is not a lifelong curse. The Expelliarmus Charm from Harry Potter’s wand can wave away the hopelessness—as long as willingness, drive, and an experienced team live beneath the Sorting Hat.