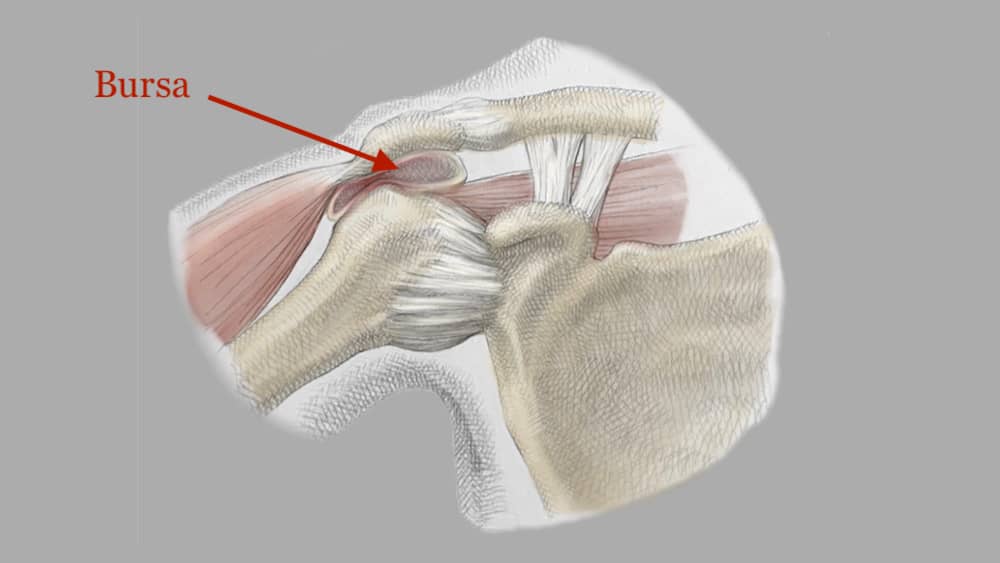
Bursitis: The Pain Outside the Joint
Joints are most commonly covered by tendons that move the bones on either side of the joint. These tendons have a sheath which, when irritated, swells, hurts, and drives us all crazy.
Original illustrated artwork by: Katerina Salsman
The sheath covering tendons is often only a few cell layers thick. It contains a tiny amount of lubricating fluid. This permits the tendons to slide easily over the bones. When the tendon or the sheath itself is injured by a fall or an overuse activity such as kneeling while roofing or playing multiple 36 holes of golf, inflammation occurs. By “inflammation,” we mean that the body rushes cells and blood vessels to the site of injury to initiate a repair response. The cells release proteins called cytokines and growth factors, as well as other compounds that switch specialized cells called macrophages to a reactive state. These cells then influence the healing cycle.
Concurrent with this injury response is the production of extracellular fluid containing the above-mentioned mixture of proteins and cells. The fluid causes the thin tendon sheath to swell. The swollen tissues around tendons are called bursae and their inflammation: bursitis.
Bursitis occurs in the shoulder joint above the rotator cuff tendons, on the front of the knee at the patellar tendon, at the side of the hip (greater trochanteric bursitis), and often at the back of the elbow. This inflammation can be shut down early in the process by anti-inflammatory drugs such as ibuprofen, ice massages, and compression. Injections of cortisone are now often avoided due to the risk of tendon rupture. Injections of anti-inflammatory growth factors from PRP, however, have been used effectively without any tendon rupture risk.
Surgery for bursitis is fraught with risk. Draining infected elbow bursae often leads to a chronic draining sinus or, worse, an infection. The same is true for the patellar bursa and the hip bursa. The shoulder responds more favorably to resection of the inflammation once other non-operative treatments have failed.
There is room for improvement in the treatment of bursitis. Better injections would shut down the inflammation more rapidly and potentially strengthen the associated tendons. Noninvasive surgical techniques using ultrasound or lasers do not yet work but have potential.
The good news about the bursae is that, treated or untreated, the inflammation almost always goes away. So while bursitis is a pain outside the joint, it is not a permanent pain in the ass.