Partial Knee Replacements
Hear From Our Patients
Partial Knee Replacement Patient from Canada (1 year post-op)People over 60 years of age with significant knee arthritis are often told to have an artificial total knee replacement. But most don’t need it. They have other options. Here is the updated information on a slice of the partial knee replacement story.
The cartilage of the knee joint—located at the end of the femur, the top of the tibia, and the undersurface of the patella—is damaged from injury and disease. The most common reasons people develop post-traumatic knee joint arthritis are fractures, loss of stability from ACL injuries, and loss of shock absorption from tears in the meniscus.
A family history of arthritis plays a role, but the causes are unclear. Are there truly inherited genes that cause osteoarthritis, or is it that you lived in the same microbiome environment as your parents and encountered some yet-to-be-discovered infectious agents that cause what we currently call osteoarthritis?
That said, the multiple causes lead to widely varying presentations of cartilage and bone damage inside the knee. Some patients have nearly complete loss of cartilage and no pain, while others have small losses that are disabling.
The solutions for knee arthritis are evolving. Many patients today try a course of physical therapy and joint lubrication injections plus anabolic factors such as PRP, mesenchymal cells (MSCs), and growth factors before considering an artificial joint replacement. Patients with mechanical symptoms (such as catching, locking, and giving way) often undergo arthroscopic “clean-ups,” where the offending tissue is removed. Other patients undergo biologic knee replacements with donor meniscus allografts, reconstructed ligaments, and articular cartilage re-grown with paste graft-type procedures. Each of these steps can be extremely helpful for the right patient at the right time.
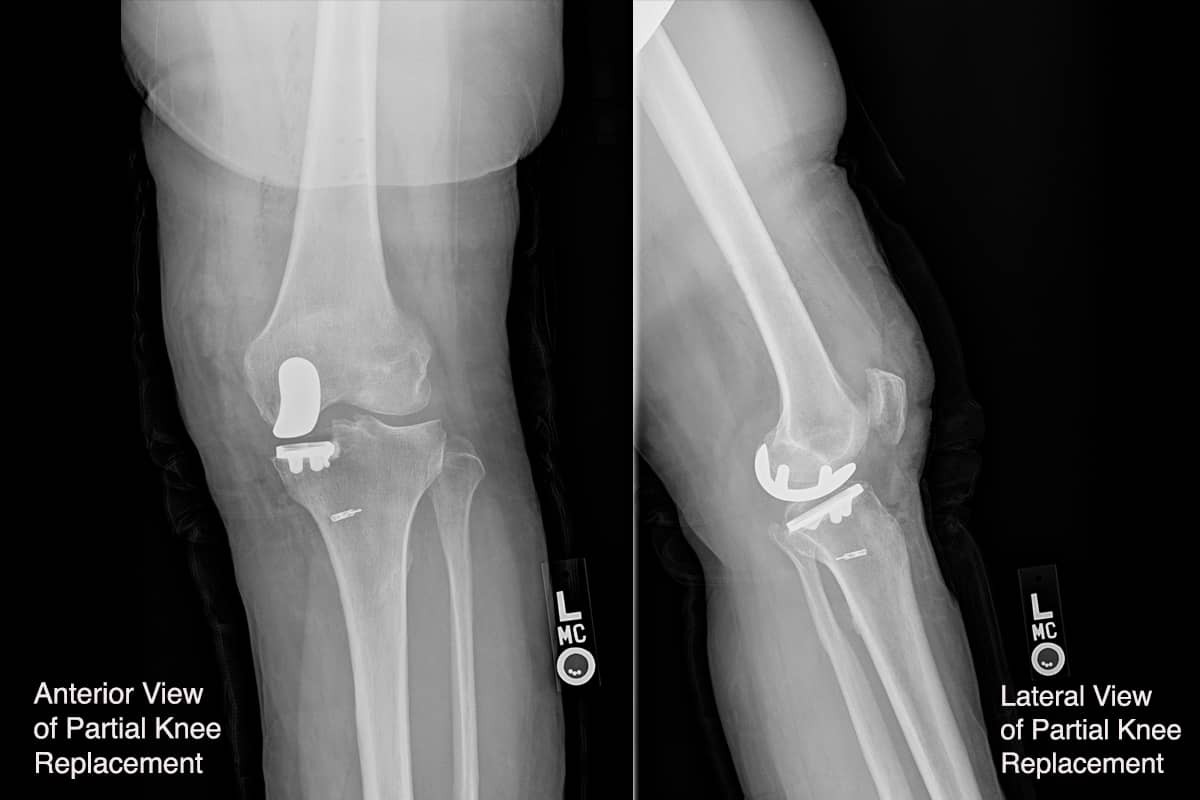
When bone-on-bone is seen on the X-ray, or in cases where the other procedures have not been sufficient, an artificial component is considered. Our bias is to resurface only the part that is worn out, so we perform partial knee replacements for medial, lateral, and patellofemoral joints far more often than a full knee resurfacing with a total knee replacement device. The success of partial knee replacements has improved dramatically with the introduction of robotic cutting devices. These devices are guided by 3-D computer models created before surgery, but require the oversight of an experienced surgeon. The robots are precise, but not very responsive to the multitude of presentations patients come in with. Tight or loose ligaments, unusual gait patterns, severe flexion or hyperextension variations all require a surgeon’s input to ensure the implants are placed in the most balanced positions. No patient is exactly like another.
Partial knee replacements heal more quickly due to the less invasive surgery and the fact that the knees feel more normal than after a complete replacement. These patients return to full sports faster; 98% say that they have “forgotten” their knee issues after 3-4 months. The main disadvantage to partial knee replacements is that they still must be cemented into place, and the cement can potentially come loose, forming a loose component in the knee—though we often see patients running long distances, hiking mountains, and skiing with abandon without problems. While the potential exists for other parts of the knee to wear out, an additional partial component can be added if needed. So, the partial knee replacement patient is not condemned to convert to a total knee.
Ideally, we would like to help patients avoid any knee surgery. The field of anabolic and cell therapy is rapidly advancing, and will hopefully diminish the need for our surgical skills. If only Pickleball hadn’t come around…
How Robotic Partial Knee Replacement Works
While we are biased to replace knees biologically, here's how recent advancements in robotic-assisted surgery technology give Dr. Stone unparalleled accuracy in placing knee replacement implants, allowing for a quicker recovery time, better range of motion, less pain medication, and greater durability for demanding activities—including running.



