Wimbledon Elbow
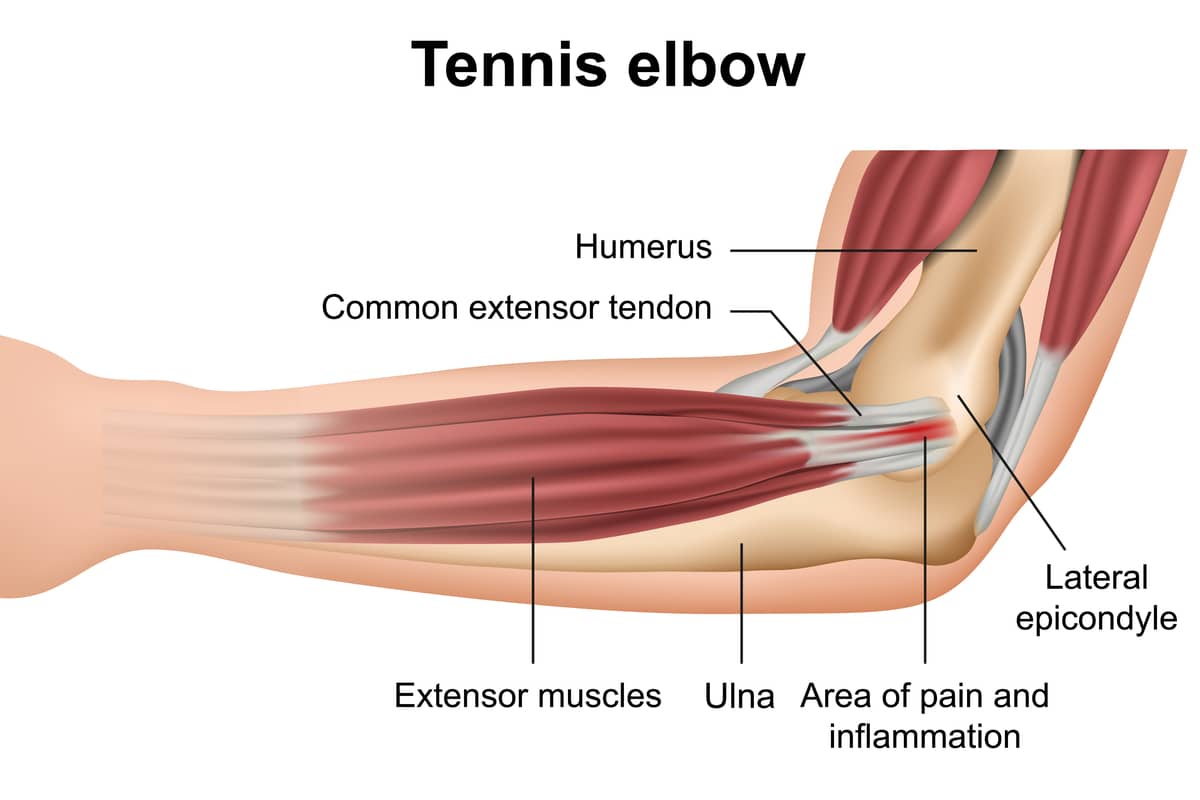
The elbow joint lies between the upper arm (humerus) and forearm (radius and ulna). It is crossed by the tendons that enable the arm to extend (triceps tendon) and bend (bicep tendon), and allow the wrist to bend (flexor tendons) and extend (extensor tendons). When excessive muscle loading occurs, these tendons can be stretched, partially torn, or ripped completely off the bone. Stretch injuries and partial tears most often heal without difficulty. But sometimes either inflammation or tissue degeneration (death) occurs leading to pain, weakness, and swelling. Here is a description of the causes and treatments.

Pictured above is Stone Clinic Patient and tennis pro Karina Torres. This article is adapted from Dr. Stone's book Play Forever.
Damage to the extensor or flexor tendons of the elbow is known as lateral epicondylitis, often called “tennis elbow.” Pain is felt at the outside or inside of the elbow joint where the tendons insert on the bone. This common injury can arise from overuse, such as playing multiple sets of tennis in one day, or from a direct injury, such as hitting a ball hard and feeling sudden pain at the elbow. Activities causing epicondylitis are not limited to tennis. They can also stem from golf or repetitive activities, such as washing windows, which can cause inflammation on the inside or outside of the elbow. The condition is painful, takes a long time to resolve, and interferes with daily activities.
One tendon, the extensor carpi radialis brevis, is most commonly the bad actor in the story of tennis elbow. While there are different theories about why this tendon, once injured, does not always heal properly, here is the basic story.
A tendon is made up of collagen fibers with specialized cells. These cells produce a range of charged molecules, growth factors, signaling factors, and other key components that keep the tissue healthy. The collagen fibers are crosslinked with chemical bridges. These permit the fibers to elongate, then return to their normal length. The fibers form ligaments that provide just the right amount of tension to permit the muscles to act appropriately.
Tension is the key to collagen function. Under tension, the collagen appropriately stretches and contracts. Without tension, the collagen degrades. A too-tight grip on the handle of a tennis racket, ax, bike bar, rowing machine—a seemingly infinite number of reasons—can cause an overstretching of the tissue. This sudden lengthening may lead to micro- or macro-tears of the crosslinks that bind the fibers together or even to the fibers themselves.
Then the interesting part begins. With normal activity, these small tears occur all the time. The body responds with increased blood flow. Progenitor cells from stem cells migrate to the site of the injury, induce macrophages (specialized repair cells) to take away the torn fibers and initiate the repair process, laying down new collagen. When done in an orderly fashion, the tissue is restored to normal and no scarring occurs. When these micro-tears occur in muscle fibers—from weightlifting, for example—the muscle heals with thicker fibers, leading to muscle building.
In the case of tennis elbow, however, something goes wrong; the reconstruction process loses its “general contractor,” so to speak. It seems there are not enough stimuli to tell the body to recruit progenitor cells and initiate the normal healing response. The tearing away from the tissue’s insertion point on the bone at the elbow releases the tension in the fibers just enough to permit the degradation process to run amok; the torn tissue just lies there and slowly degrades. The chemical by-products of this degradation lead to the stimulation of pain neurons. If allowed to continue, cell death and permanent collagen fiber degeneration can occur.
Tennis elbow can be the kind of tearing that heals naturally or the ugly kind that leaves weakened scar tissue and chronic pain. Treating the injury in a way that helps increase the probability of normal tissue healing is the goal. The classic treatment for tennis elbow—cortisone injections— reduces the inflammatory agents at the site of the injury, does nothing to stimulate healing but does relieve the pain in fifty percent of the cases. Cortisone sometimes makes the problem worse by shutting down cell metabolism and weakening the tissue.
Soft-tissue massage to the damaged area breaks down scar tissue and stimulates the production of more collagen through a combination of cell stimulation and collagen fiber cycling. New collagen is laid down at the site of the injury. If careful stress is applied (in the form of gentle exercises), the collagen fibers line up along the lines of stress, leading to healthy healing of the tissue. Bracing the wrist, to decrease the distance the tendons are stretched, often helps—as does an elastic band wrapped around the forearm. If the joint is immobilized, however, scarring is more likely to form—with weakened tissue as a result.
Ice can reduce both pain and inflammation in tennis elbow. The relief is limited, however, as the real issue is not inflammation but tissue degeneration. It takes a new stimulus to remove this relatively dead tissue. This stimulus can take three forms: surgical, where the tissue is physically removed and sewn back to the proper length; manual, where massage therapy or shock therapy stimulates the repair; or chemical. Chemical stimulation today is best performed by the injection of growth factors. These injections change the cellular environment surrounding the degraded tissues, recruit progenitor cells, and stimulate healing. In multiple studies comparing the therapeutic results of cortisone injections to growth factors extracted from blood platelets, the growth factors appeared to be more effective. In another study, collagen fibers were restored to their normal mixture of small- and large-diameter fibrils under the stimulation of birth-tissue-derived growth factors and cells.
If not cured immediately after it appears, tennis elbow has a nasty habit of becoming chronic and painful. Attacking it early and often to prevent the death of the tendon tissue may be the best approach. It is always much easier to cure the injured than to resurrect the dead.
For more guidance on avoiding chronic injuries, check out Dr. Stone’s book Play Forever: How to Recover from Injury and Thrive, on Amazon now.