Tendonitis or Not?
Hear From Our Patients
Surfers Returns from Ruptured Achilles with Percutaneous RepairTendonitis is a pain. Whether at the elbow, knee, shoulder, or ankle, a painful tendon is often called tendonitis. Sometimes, it actually is—but often not.
Tendons connect muscles to bones. As the muscle contracts, it pulls through the tendon to move the bone in a joint. The tendon is made up of dense collagen fibers, crosslinked with glucosamine or charged sugars. Lubricants (primarily hyaluronic acid) help the tendon—which often rests within a thin sheath—to slide. Each of these connected components presents an opportunity for injury, disease, and the pain you feel when the tendon hurts.
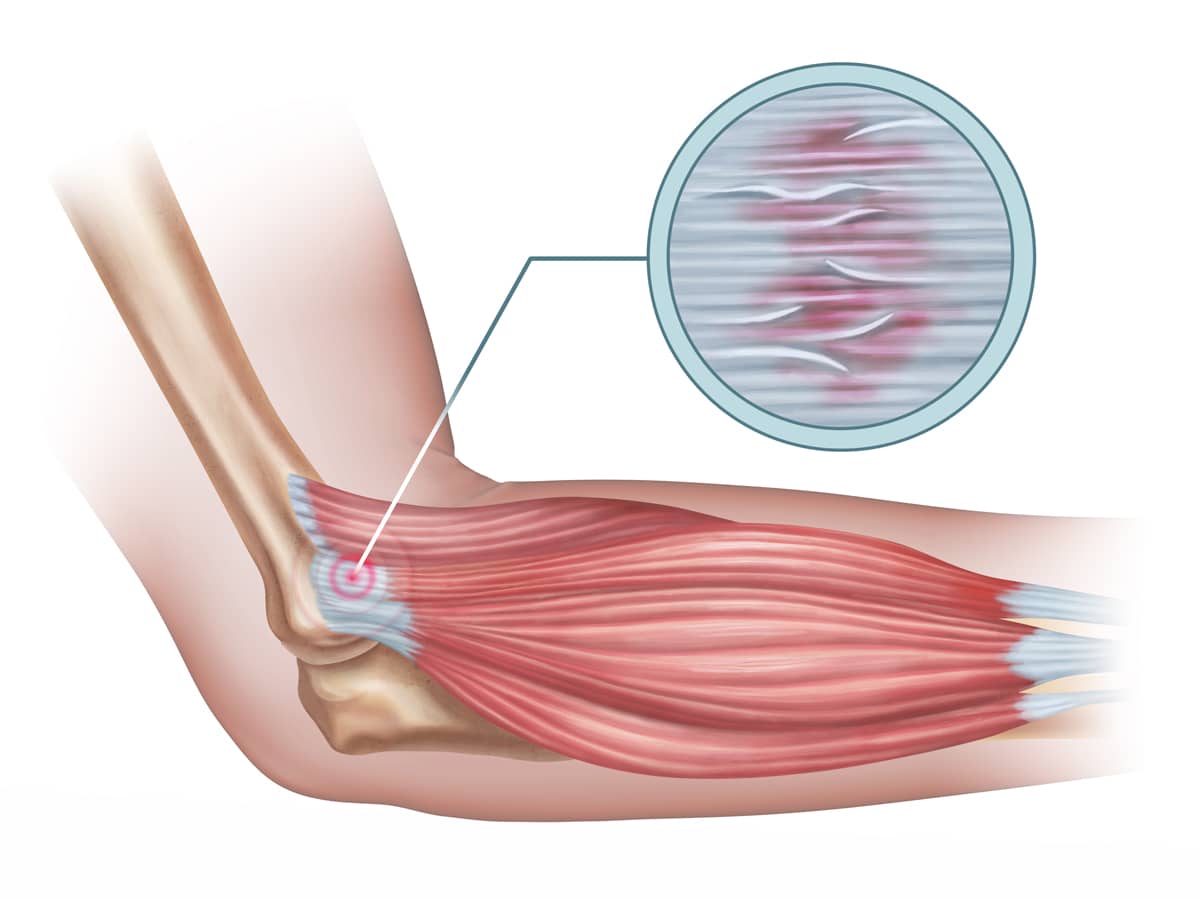
Collagen fibers stretch naturally, to a degree. However when a sudden elongation occurs, past the point of elasticity, the fibers tear. The degree of tearing determines the seriousness of the tear. A mild stretch may involve only a small percentage of the fibers, while a complete tear involves 100% of the fibers.
Upon injury to the collagen fibers, the surrounding nerve fibers send pain signals to the brain. This acute injury, characterized by swelling, is called inflammation. The healing phase of these partially torn fibers is usually called tendonitis, with the suffix “-itis” meaning inflammation.
The treatment for this is a combination of soft tissue massage, icing, stretching, and sometimes bracing and straps. Anti-inflammatory drugs such as ibuprofen quiet the pain and swelling, but have been shown to cause abnormal collagen formation, thus possibly weakening the healing process. Newer therapies focus on injections of anabolic therapies, such as platelet-rich plasma (PRP). PRP has anti-inflammatory properties, and it stimulates cellular healing and collagen formation as well. Electrical stimulation, shock wave therapy, needling, and magnetic therapies have all been used to accelerate this healing, with varied data on their efficacy.
Chronically torn fibers continue to hurt. This may be due to chronic inflammation, which sometimes responds to classic anti-inflammatory therapies (but often does not). Chronic tendonitis, in fact, may not be an “-itis” at all. This may be because the torn fibers, instead of healing properly, have degenerated— forming a relatively dead area of the tendon. Degeneration does not respond to anti-inflammatory therapy. Often, only surgical excision of the dead area—and the suturing together of the healthy areas of the tendon—will cure the pain. The hard thing for patients and doctors to determine is whether the issue is chronic inflammation or degenerative dead tissue.
Anyone who has suffered from golfer’s and tennis elbow, patellar or Achilles tendonitis, or months-long rotator cuff pain has the same question: What do I do to heal this and resolve the pain? The answer lies in making a clear determination: -itis, or dead? Therapy or resection and resurrection?
What's the Best Way to Fix a Ruptured Achilles Tendon?
At The Stone Clinic, we repair Achilles tendon ruptures without open surgery using the Percutaneous Achilles Repair technique. Over the past 30 years, Kevin R. Stone, MD, has refined this approach to eliminate the need for a large incision, preserve growth factors that accelerate healing, and reduce infection risk. Here’s how.


