Chicken Soup: What’s New in the Field of Cartilage Repair?
The science of cartilage repair for joints is in full swing. There is a frenzy of activity around stem cells, growth factors, exosomes (small packets of growth factors), and all forms of stimulation therapies. And the matrices or patches that those factors are placed on vary widely. The bottom line is that no one factor does it all. Here is the latest update on what needs to go into the chicken soup of tissue repair to make you well.
Injuries to tissues involve tearing of the fibers, bleeding into the damage site, tissue swelling followed by a coordinated repair response dance that must go well for tissue restoration to occur. If not scarring forms or tissues don’t heal at all. The cartilage in human and animal bodies is unique in that it does not have blood vessels, so injuries to it don’t cause bleeding. In fact, the injuries most often do not heal at all.
The articular cartilage is the white, shiny surface on the ends of all bones in joints. It is dense tissue, with a glass-like (amorphous) matrix that has few cells, a small amount of carbohydrate sugars, and lots of water. It is bathed in synovial fluid, a joint fluid that contains hyaluronic acid. This lubricant permits the joints to have a super low coefficient of friction, five times slicker than ice-on-ice.
When the cartilage is injured this friction increases, leading to more wear, and eventually arthritis: the crippling disease of exposed bone, inflammation, and joint pain.
Nature probably didn’t design a system without some self-repair, but we as orthopaedists and scientists haven’t yet figured out the best ways to harness that system—and our patients do sports that impact the surfaces far beyond the normal loading levels. In the past, when the joint surfaces were significantly injured (and sometimes even today), surgeons removed the damaged tissues and told patients to wait until they were older for artificial joint replacement.
But now we have entered a new era—what I call the “anabolic era” of sports medicine. We put tissues back into joints, and we stimulate them to heal with novel forms of cells and growth factors. Here is what is hot and what is not in this active field.
In the past, there were several major techniques to repair the injured cartilage. These included shaving it away, microfracturing it to elicit a healing blood clot, injecting cartilage cells under a new flap of periosteum or bone tissue, or using plugs of cartilage and bone either from another part of the joint or from a donor. Today, matrices of collagen patches and other materials are being used to hold cells and growth factors onto the site of cartilage injuries. Our preferred technique involves using a paste of cartilage and bone packed into the defect in the cartilage, after it is super microfractured or morselized into a fresh fracture.
Each of these techniques has demonstrated some success, but none have been perfect. All take too much time to heal and some involve expensive implants. To make them better, injections of accelerants were developed.
Growth factors from platelets (PRP), bone marrow (BMAC), and fat are being concentrated in various tabletop devices in the operating room. All contain factors that both promote growth and attract stem-cell-derived progenitor cells to the site of injury that produce additional factors that drive healing.
What is evident at this point is that cartilage repair takes a village. The environment for healing must include the right materials, the stimulation of the correct cells at the optimum moments, and the physiology and psychology of the patient to accept and promote a healing process. When any one of these factors is not present, the process of healing is incomplete. In the case of cartilage, unless all the systems are marshaled to work together, the injury and subsequent repair effort lead to arthritis.
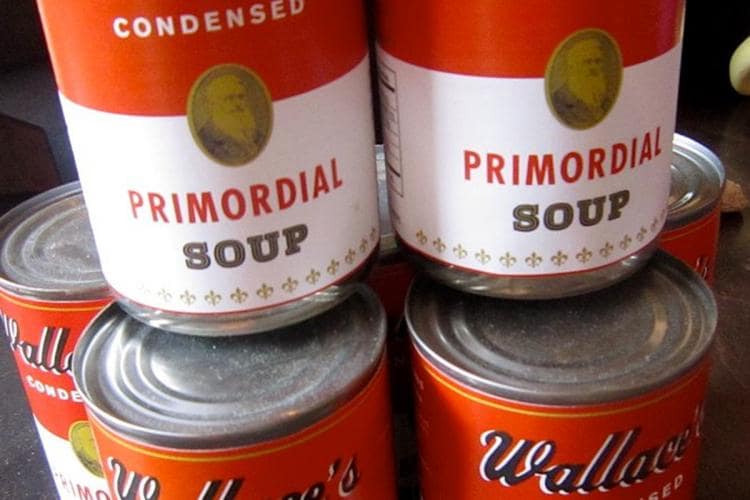
As our grandmothers figured out, when you treat a cold with chicken soup you warm the body, calm the mind, and promote healing. The primordial soup surrounding cartilage injury repair needs a modern version of our grandmothers’ wisdom.
