Articular Cartilage Repair…What Is It?
The articular cartilage is the bearing surface covering the bones in all of our joints. It has remarkable biomechanical properties. Once injured, however, it surprisingly lacks the ability to heal on its own. The following describes just what articular cartilage is, and the surgeon’s options for repairing, regenerating, and replacing this tissue.
Articular cartilage is hyaline (i.e., glass-like): an amorphous gel with few cells scattered through its matrix. It has no blood vessels, no nerves, and no lymphatics. Yet the matrix does have a complex sugar, called glycosaminoglycan, that absorbs water and lubricants and expresses them when force is loaded onto the joint. This combination of components permits the surface to be five times slicker than ice on ice—unless it is injured.
Once injured, the lack of self-repair ability causes the tissue to wear down, gradually, to the underlying bone. The injury can arise from a number of causes: a direct blow in sports; prior surgical removal of the meniscus shock absorber, which then concentrates weight-bearing forces in a small area; a tear of the ACL, leaving the knee unstable; or the disease of arthritis, which eats away at the cartilage.
In all of these cases, the worn-away hyaline cartilage exposes the underlying bone. The bone then becomes vulnerable and undergoes degrading changes. Repair options focus on three areas:
One: Smoothing down surrounding frayed tissue—a procedure called a chondroplasty—and micro-fracturing the exposed bone. This generates a temporary fibrous tissue; a sort of healing Band-Aid.
Two: Engendering a robust healing response. This is done by aerating the exposed bone and using a combination of marrow cells to provide a stimulating matrix. This matrix acts as a regeneration trellis for new cartilage.
Three: Replacing the missing cartilage with a plug of intact bone and cartilage from either the patient or a donor.
Of those choices, we prefer an enhanced version of choice number two: a procedure called articular cartilage paste grafting.
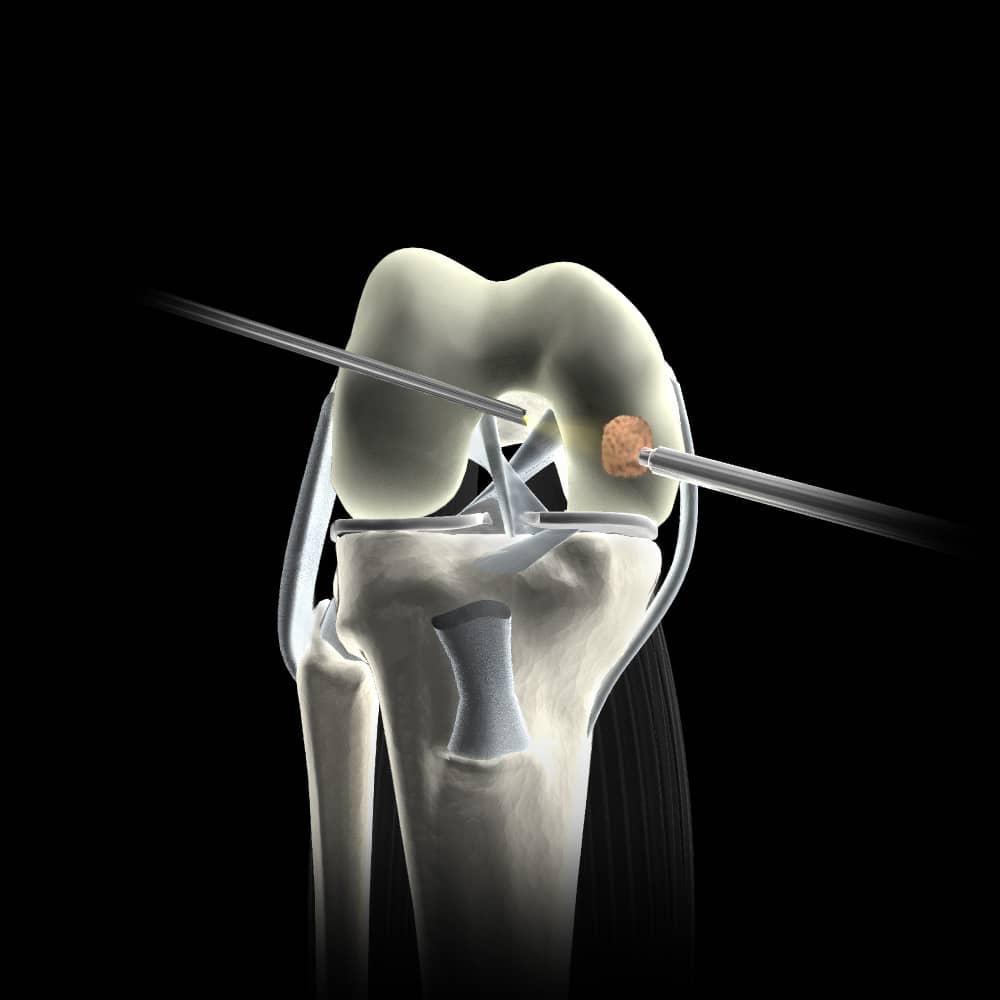
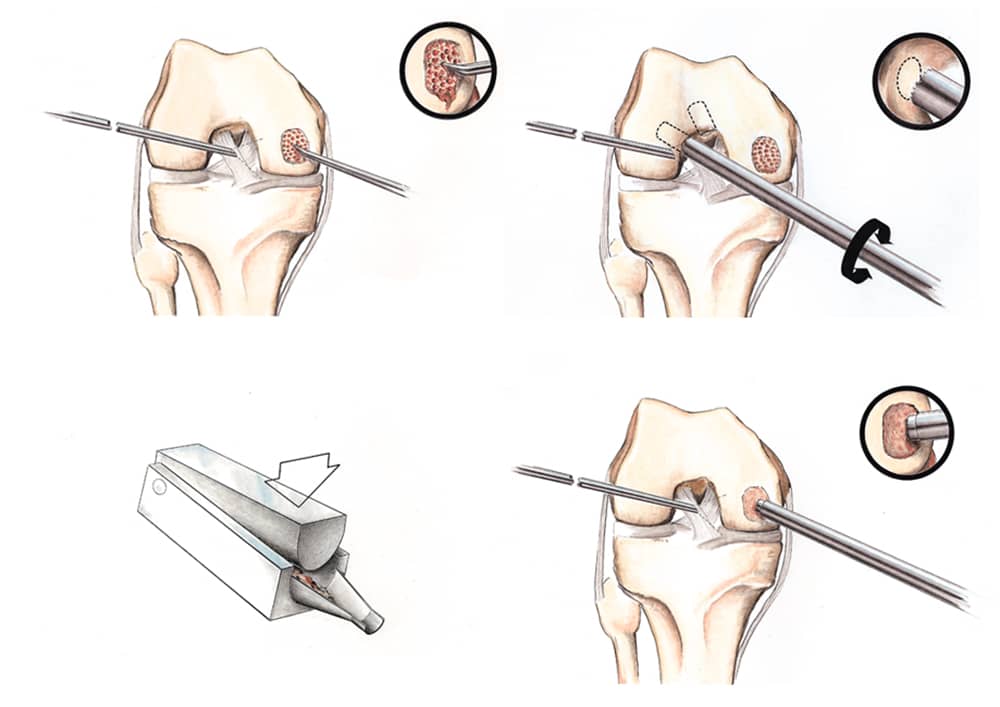
The paste graft technique works by combining the body’s natural strengths with skillful intervention. Using a technique that causes a significant fresh fracture at the exposed bone site, we stimulate the release of marrow cells. Those healing cells rush to the site of injury. There, they encounter a paste composed of healthy articular cartilage and bone. This paste has been made from a core taken from the intercondylar notch of the knee (a place where we know it has the ability to regrow), and impacted into the prepared area. Independent clinical studies have shown that the introduction of this paste stimulates the cells of the articular cartilage, causing them to express a more robust self-healing matrix.
The other options—using scaffolds made with preloaded cells (MACI) or artificial scaffolds with bone substitutes (or ground-up donor cartilage)—do not induce the same level of healing response produced by paste grafting.
The strategy of articular cartilage paste grafting has worked well in our clinic for more than thirty years. We have long-term outcome studies demonstrating its efficacy. Useful for both acute injuries and arthritis, the technique is a one-step arthroscopic process. In addition, it doesn’t burn any bridges: The repair tissue produced by this technique is either normal-looking articular cartilage or a mixture of normal areas and fibrous cartilage. Paste grafting is the only technique indicated for the arthritic knee and can be combined with meniscus replacement when required.
The journey to complete healing does not end with surgery. It is crucial to provide post-operative motion to the grafted areas since motion tells the healing cells to become cartilage rather than bone or scar tissue. A continuous passive motion machine (CPM) is used for four hours each day (or night), crutches are used to protect the repair tissue for one month, and a specific intense exercise program begins the first day after surgery. The goal is to get in a good aerobic workout every day, as this increases the flow of blood, testosterone, pheromones, and adrenaline: all helpful components of the healing response.
The new tissue matures over the course of a year, improving in durability and pain relief. By three months after surgery, though, the patient can return to most activities. Our goal for cartilage repair is to return the patient to their full range of activities, including sports, whenever possible.

