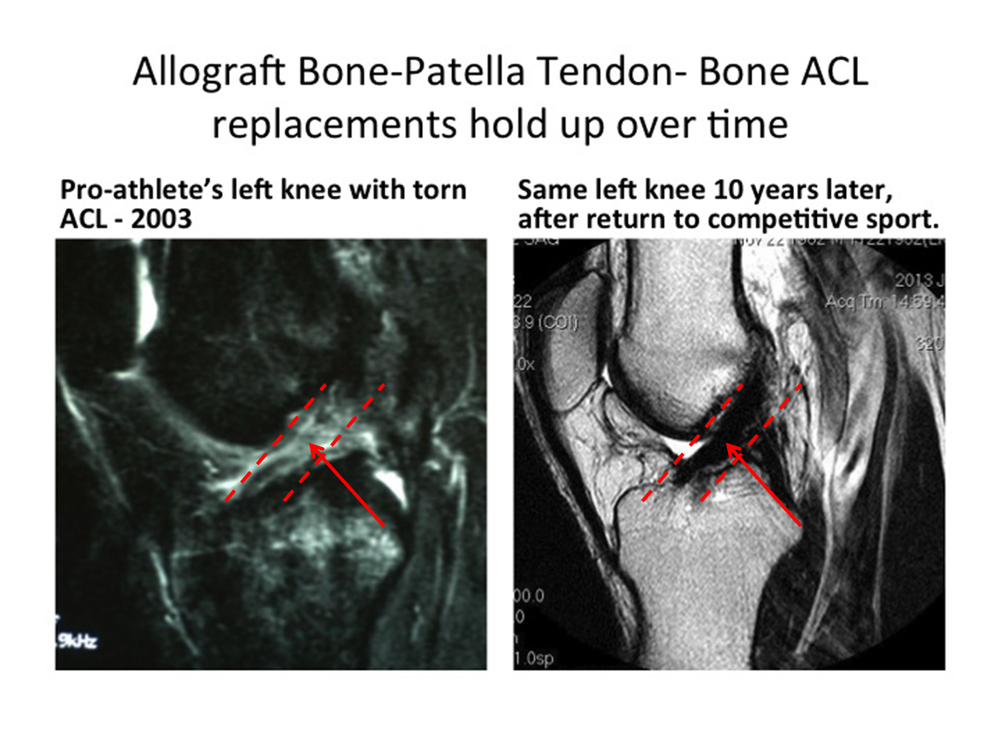
Donor tissue best for ACL reconstruction
In treating an ACL rupture, surgeons have a choice about whether to harvest a patient’s own tissue from their patellar tendon or hamstrings or instead to use donor tissue from a tissue bank.
This choice is a hotly debated topic in the orthopedic community. Here’s why we opt for donor tissue.
ACL graft failure
We saw a patient this week whose ACL replacement graft (performed by another clinic) had failed. The failure was due to incorrect placement of the ACL on the femur and also a failure to recognize that the ligaments in the corner of the knee had been injured as well. Unfortunately, in addition, the previous surgeon had used the patient’s own hamstrings, which left this world-class athlete slightly weaker in knee flexion. At The Stone Clinic, we have extensive experience in revising failed or reinjured ACLs. What we did differently for this patient, as with others, is we first recognized the injury to the posterolateral corner of the knee and reconstructed it with a donor tendon. We also placed a new donor ACL in the correct anatomic position on the femur while preserving some of the previous surgeon’s graft. Failure to recognize the corner injury and misplacement of the ACL are the two most common reasons for ACL graft failure.
Patient’s own tissue vs donor tissue
The ACL is the key guiding ligament of the knee joint. Unfortunately, an ACL rupture is an all too common injury in sports. Treatment options vary. Some surgeons use the patient’s own tissue from their patellar tendon or hamstrings, some use donor tissue from a tissue bank. It's a controversial choice. Robbing Peter to pay Paul is clearly not the future of any treatment; moving a patient’s own tissue from one place to another weakens the knee and permanently increases the risk of arthritis. On the other hand, studies have shown that donor tissue from a bank produces mixed results. Thus many surgeons continue to take tissue from the patient in all cases or refuse to use allografts in young or athletic patients.
Flawed studies
Yet, the scientific literature on allograft ACL reconstruction is unreliable. Even the best studies published so far include a vast array of donor (allograft) tissues: from young and old patients, from hamstrings, Achilles tendons and patella tendons, and from un-registered banks with variable exposure to radiation. With such a mixed bag of tissues, it’s no wonder the results are mixed.
Our strict criteria
At The Stone Clinic, we come down firmly on the side of using allograft tissue. We believe donor tissue to be the best choice in all cases but ONLY if these strict guidelines are followed:
The tissue is:
- From a donor less than 40 years old.
- Prepared at a nationally registered tissue bank and processed to assure sterility, limiting radiation to below 2 mRads
- Bone-patellar tendon-bone
- Surgically implanted anatomically with high accuracy
- Fixed with secure fixation
- Rehabilitated with optimal strengthening programs
Here’s our reasoning:
1) Young donor tissue
Tissue biomechanical characteristics degrade 1% per year after 20 years old. So a 40-year-old’s tissue is 20% lower in strength characteristics than that of a 20-year-old. The use of young tissue really does matter. Many studies don’t list the age of the donor.
2) Minimal radiation
Tissue banks use a wide variety of sterilization procedures, some of which have not been thoroughly tested for their effects on biomechanical properties. When a bank’s process is not ideal, they may finish the sterilization with radiation. Radiation above 2 mRads significantly decreases the strength of the tissues. Even when the tissue banks report that their process uses a lower dose, it cannot always be trusted as thicker tissue and thinner tissues may receive widely different doses of radiation when in the same treatment chamber. A dose range, not a specific dose, must be reported with the upper end of the range below 2 mRads.
3) Patella tendon
The strongest tissue replacement for the ACL has been proven to be the patellar tendon with bone blocks at each end, called bone-patella tendon-bone. Except for shortages in donor supply, there is really no reason to use weaker tissue. Some tissues are altogether unsuitable, such as the Achilles tendon, which is a muscle to bone construct, naturally designed to stretch considerably before rupture. It makes no sense to us to use a stretchy design for a ligament you don’t want to stretch.
4) Accurate placement
The number one cause of ACL failure is the errant placement of the ligament by the surgeon. Surgical skill and the accuracy of placement of the new ligament determines much of its success. The key to accurate placement is the anatomic insertion of the native ligament. Some insertion techniques such as the “transtibial,” which uses a single drill hole from the tibia to the femur, may be easier but have been shown in multiple studies to be much less likely to produce anatomic holes for ligament insertion than “two-incision” techniques. There is rarely justification for non-anatomic placement
5) Secure fixation
Fixation of the ACL replacement has been repeatedly shown to be highest and stiffest when bone is fixed to bone at both ends of the graft. Thus a bone-patellar tendon-bone construct provides the best graft and the best opportunity to fix the graft securely. Additionally, bone healing to bone is stronger than tendon healing to bone.
6) Optimal rehabilitation
Lastly, rehabilitation should return the knee to a full range of motion equal to the opposite leg. The patient should continue PT through strength training and end up stronger than they were before they were injured, with balance and coordination restored. The way to achieve this is to with an intense, rehabilitation program that is individually designed for each patient focusing on their whole body and not just their leg. Our StoneFit program uses many of the CrossFit exercises customized to ACL rehabilitation.
At The Stone Clinic, more than 90% of our patients are able to return to full sports with a stable knee.
