Bone-on-Bone to Peak Performance: How One Athlete Solved the Knee Arthritis Problem
My name is Myles Mourdant. I’m 52 years old, and I’m now about a year and a half post-operation — a point where I’ve had time to reflect on how far I’ve come. I’m a businessman living between Monaco and France, and sport has always been a central pillar in my life. You don’t always realize how much your life revolves around sport until someone tells you that you may lose it.
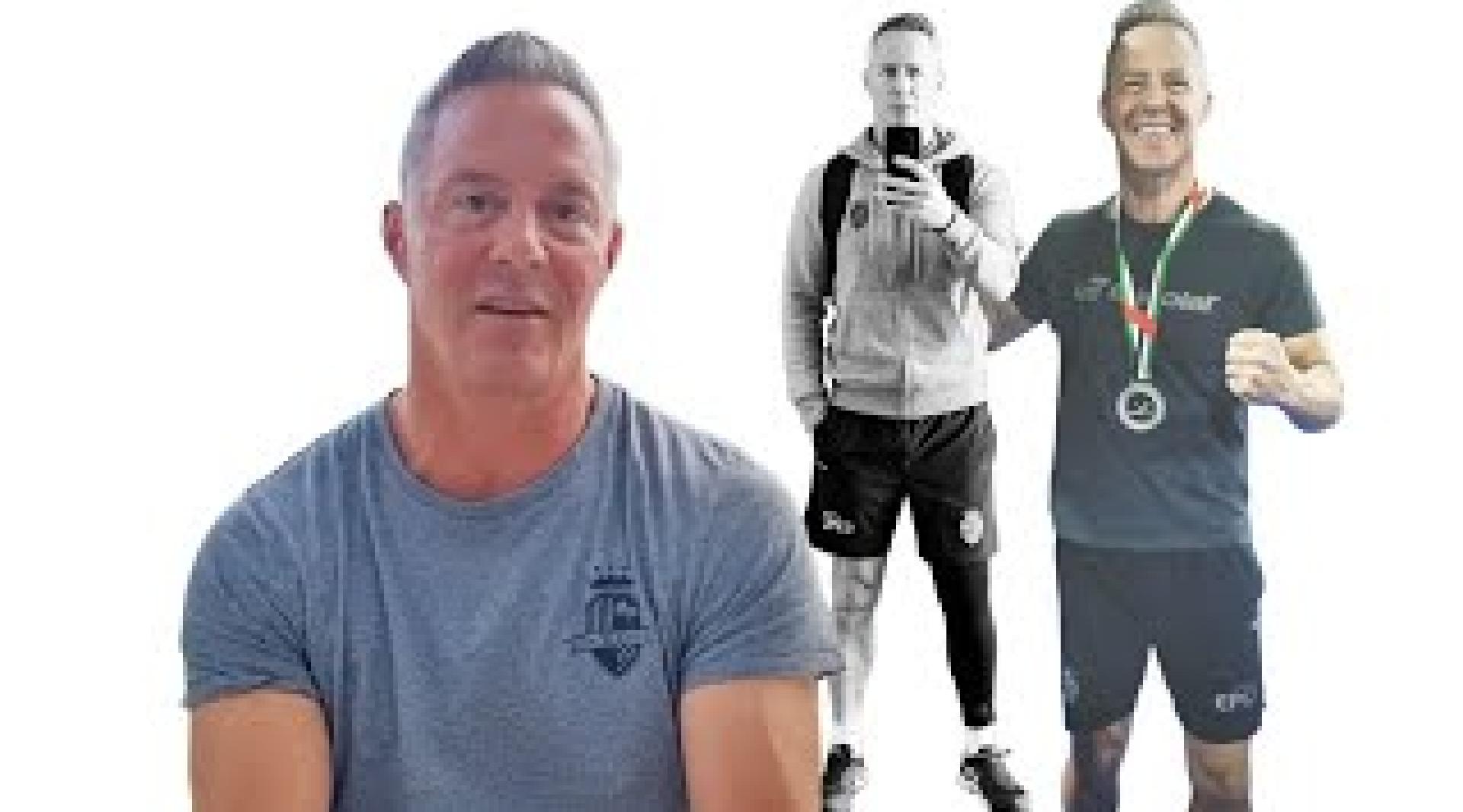
I’ve always been the kind of athlete who is reasonably good at several things, even if not exceptional at any one discipline. Sport has always grounded me. At my competitive peak, I won a bronze medal driving a bobsled in the British Bobsled Championships. These days, padel is my main sport. While it’s still growing in the U.S., it’s huge in Europe and is one of the fastest-growing sports in the world.
Because I’m now over 50, I qualify for the senior circuit, and I had been working toward competing for the Great Britain Seniors team. Unfortunately, an old injury from 20 years ago caught up with me — a medial meniscus tear in my right knee that was trimmed at the time. As Dr. Stone would say, that was not the ideal approach, and two decades later the consequences finally appeared. I was playing padel five days a week and training three days a week — around 10–12 hours of intense sport — when my knee began to deteriorate rapidly.
The pain progressed quickly. Within two to three weeks, I could no longer walk up or down a flight of stairs. It turned out that the joint surfaces had finally begun to make contact, and I was stripping the articular cartilage from my femur. After getting an MRI and X-rays and consulting with three surgeons within a week, I was told the same devastating message: “You’re done. Stop sport. Wait ten years until you’re 60, and then you can have a knee replacement. We don’t do those under 50.” Surgeons in Monaco, France, and even those I spoke with in the UK delivered essentially the same message. Some suggested hyaluronic acid or PRP, but once the articular cartilage is gone, those treatments aren’t enough.
It was crushing. I remember thinking: Do I really have to give up sport now? Instead, I threw myself into researching options. For two weeks, I spent five or six hours a day reading everything I could. I kept coming back to Dr. Stone’s work. I read every paper of his I could find, and it was the first time I felt there might be a real solution — that sport didn’t have to be over for me.
Eventually I reached out. His team was incredibly efficient and helpful, and within three days I was on a call with Dr. Stone. I had prepared around a hundred questions. The call lasted eight or ten minutes, and I got through maybe three of them. Each time I asked something, he simply repeated: “I can help you. Come here and we’ll fix this.” He asked what my goals were, and I told him: I want to sprint. I want to play sport at the same level. I want to compete at the highest level for my age in padel.
His response: “I can fix that.”
I remember getting off the call thinking: Either he’s the world’s most confident salesman — or he truly means it.
He meant it.
I booked the operation for three weeks later. The original plan was a meniscus transplant and a paste graft. But when I arrived in San Francisco, we repeated the imaging — MRI, X-rays, and a 3D scan — and it was clear that even in those three weeks, despite resting, I had shredded a significant hole in the articular cartilage on my femur. Dr. Stone explained the situation honestly: we could try the original surgery, but a partial knee replacement was now the better option. His confidence in the results was reassuring.
He encouraged me to speak with the physical therapy team on-site — a huge benefit of his clinic. They asked detailed questions about my sport, my training load, and my goals. After evaluating everything, they agreed that although I could attempt a meniscus transplant and paste graft, my profile made me an excellent candidate for the partial knee. It offered faster recovery and extremely strong outcomes. In hindsight, I’m thrilled that this was the route we took.
The operation was four hours. The hospital is about half an hour from the clinic. I was there a total of five hours, including recovery. Incredibly, I walked out on crutches the same day.
The next day, I began two physical therapy sessions. I deliberately stayed in the U.S. for three weeks so I could work daily with Dr. Stone’s team, who are literally next door to his office. He stopped by frequently to check my progress. I used crutches for five days. The first week was focused on managing swelling, compression, and carefully working on range of motion. The third day is typically the hardest as some of the surgical pain medication wears off, but nothing was unmanageable.
Flexion was the most challenging part for me. I worked hard on stretching protocols and elevation, and as long as you follow the program, recovery moves steadily forward. When I returned home, I continued compression therapy, used red light therapy for the scar — which is now barely a pencil line — and kept building strength.
By eight weeks, I had regained the two centimeters of quad mass I lost. By six months, I was 95% recovered in the surrounding musculature. Now, both legs look and function equally. You do lose some sensation around the incision because of nerve disruption, but that gradually returns; even at a year and a half post-op, it continues to improve. It’s never painful — just a bit different.
The physical milestones that followed were extraordinary.
At seven weeks, I went from crutches to plyometric bounding.
At three months, I was back on a padel court — and even achieved a net jump, a personal goal I thought would take a year.
At six months, I won second place in the European Padel League tournament in Dubai.
That same weekend, I beat the British No. 1 and a French national team player in friendly matches.
I also skied that winter — all with zero pain.
The best part is this: when I play sport now, I never think about my knee. There is no hesitation, no protected movement, no subconscious fear. I can lunge fully onto my operated knee, rebound from it, sprint off it — exactly like before. If anything, my left knee sometimes feels like the “weaker” one because the right is performing so well. And of course, if you play a lot of sport you can still get normal soreness or lactic acid in both knees, but that’s just sport — not joint damage.
My conclusion is simple: if someone tells you there’s no solution for your knee, get a second opinion from Dr. Stone. Send him your MRI and X-ray. If he says he can fix it, he can. And if he says he can’t, then it’s likely true — but his philosophy is the opposite of “give up sport.” He wants you skiing and playing into your 80s. And he lives that philosophy himself.
I’m extremely grateful for what he and his team have done for me.
Thank you.
Myles M. Profile
Myles is a lifelong athlete whose active life came to a sudden halt when a rapidly worsening knee left him unable to walk up or down stairs, let alone continue competing in padel tennis at the senior international level. He had medical consultations in Monaco, France, and the UK, and received the same message: “Stop sports and wait a decade for a knee replacement.”
Myles refused to accept this limitation, and his search for a better solution led him to Dr. Stone and The Stone Clinic. Here, he underwent a robotic-assisted partial knee replacement that could support a full return to sports.
Eighteen months later, he is fully back to sport: lunging, sprinting, and competing pain-free at an elite senior level. He’s skiing, winning padel tournaments, and feeling faster and more confident than he has in years. Way to go, Myles!