Male Hormone Replacement Therapy
One of the few areas of medicine where women have been paid more attention than men has been the field of hormone replacement therapy.
It is now widely understood that as women age, they benefit from estrogen and progesterone by experiencing less muscle loss, less bone loss, better mental acuity, and more healthy, lubricated skin everywhere. While it is important for women to start the replacement within 10 years of (or even before) menopause, the benefits far outweigh the risks in almost every study. Only a distorted—and, frankly, dishonestly reported—breast cancer study in 2002 held back replacement therapy.
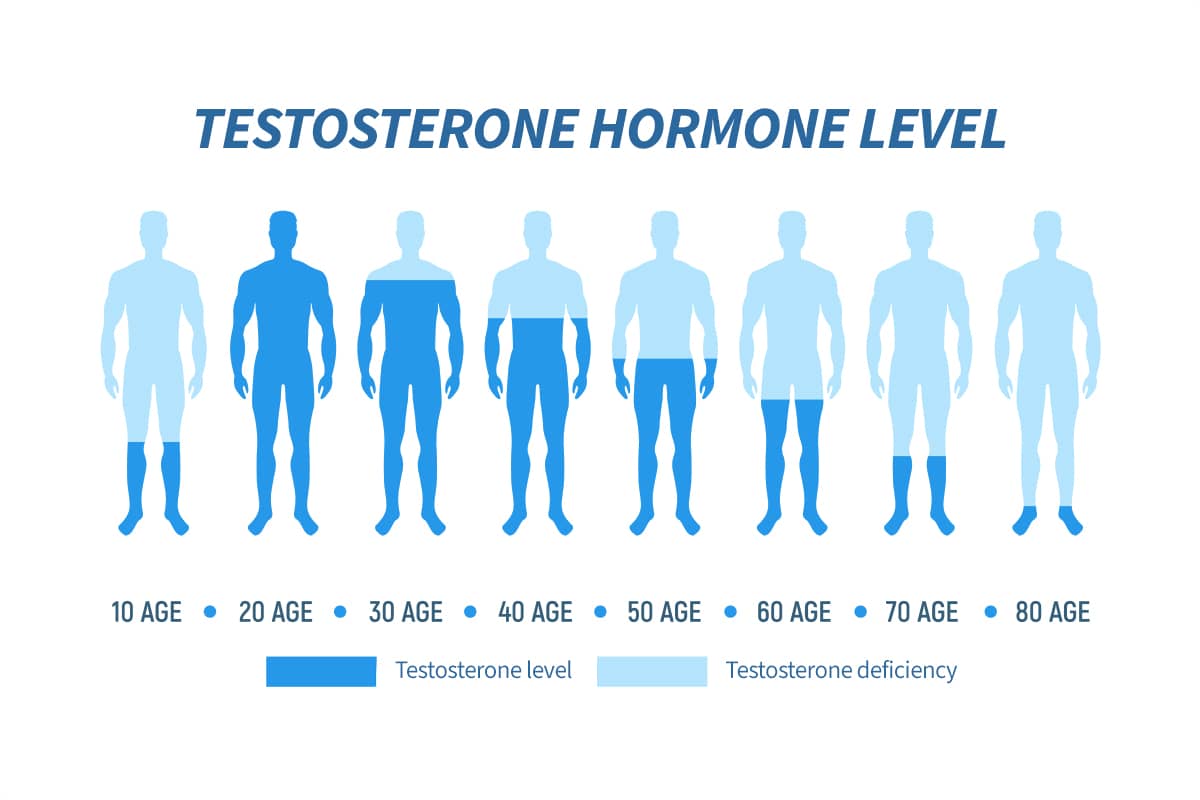
Men lose muscle, bone, and sexual performance as they age, with dramatic consequences as well. It is roughly estimated that 70% of men age 70, 80% of men age 80, and 90% of men age 90 have significant erectile dysfunction affecting their psychosocial dynamics. Muscle and bone loss, meanwhile, lead to imbalance, falls, hip fractures, and loss of life.
Since men as well as women are losing replaceable tissues due in part to replaceable hormone depletion, why are we not replacing the losses?
The field of male hormone replacement therapy took a major hit from the 1960s to the 1980s with the abuse, by weightlifters and bodybuilders, of massive doses of testosterone and synthetic substitutes. At those doses, liver disease, shrunken testicles, and male breast enlargement—due to testosterone’s natural conversion to estrogen—soured both the public and the FDA on testosterone as a legitimate therapy.
When HIV came along in 1980, physicians finally became comfortable using testosterone to treat the viral-induced, muscle-wasting disease. Unfortunately, it was too late for some of the best synthetic versions of testosterone, which were designed to be anabolic—i.e., without the feminizing effects of testosterone alone. Banned by the FDA, they still remain off the market. So, testosterone alone, in various formulations, is now the only real choice. And testosterone is tricky to use properly. For instance, testosterone blood levels vary during the day. To get an accurate assessment, both the bound and free testosterone must be measured between 8-10 a.m., and the free testosterone assessed by only one of the three available measuring techniques, called equilibrium dialysis. Most labs will use the less expensive method by measuring total testosterone, sex hormone-binding globulin (SHBG), and albumin levels, then use a calculation to estimate the free testosterone concentration. All of these components of the blood must be drawn for the calculation to work. What the true range of “normal” is for each person, and what level is required to offset the decline due to aging, is in debate.
Despite all the television ads about “low T,” men are losing a wide variety of poorly studied hormones and not receiving rational guidance. Fortunately, several tsunamis are occurring. For one, the focus on longevity has brought money and science back into studying not only testosterone, but other hormones as well. Peptides (small chains of amino acids) have been shown to be both enormously effective at weight loss (think GLP-1), in modulating diabetes and, in smaller doses, effective as anti-inflammatories and anti-depressants. BPC-157, a widely used but poorly studied peptide, is ubiquitous in gyms and longevity centers around the world today. These peptides act like hormones, with a wide range of mostly beneficial physical, psychological, and emotional effects.
When we look at injured athletes, we think about how to repair their injuries and return them to sports fitter, faster and stronger than they have been in years. When we look at people aging, both male and female, we are now asking how we can modulate their decline with a combination of exercise, nutrition, stress reduction, and hormonal replacement therapy. True, this entire line of research should have been obvious years ago—but better later than never.
