Paste Grafting and Stem Cell Cartilage Repair in 2023
Articular cartilage covers the ends of all bones in joints. It is five times as slick as ice on ice and has no blood supply. Only a few cells are scattered through an amorphous, water-filled matrix. When injured it often fails to heal. It presents a challenge that many of us have tried to solve. Here is a brief history of our approach.
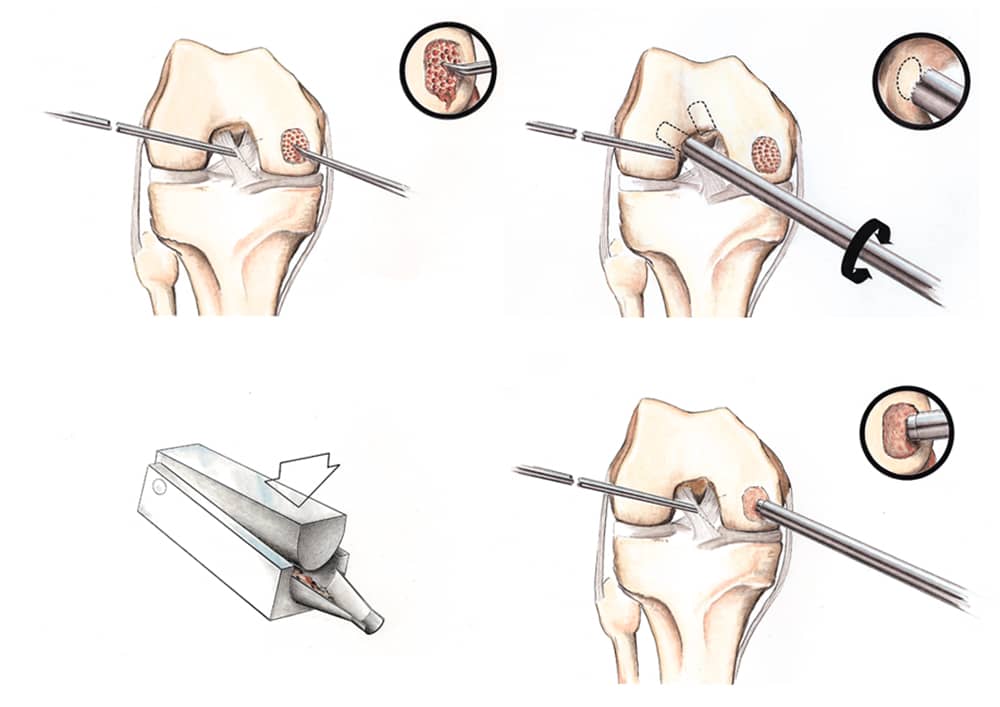
Diagram of the articular cartilage paste graft technique used by Dr. Stone to stimulate cartilage regrowth and healing
We started with blood. In orthopaedic sports medicine, we knew by the 20th century that fresh blood was critical for all types of healing. Cartilage injuries, which were difficult to heal, could be temporarily cured by drilling into the underlying bone and bringing forward fresh marrow blood.
Robert Salter, MD, demonstrated that fresh marrow clots could be induced to form cartilage (as opposed to scar tissue or bone) by the application of continuous passive motion. Thus, CPM machines were created, designed to move joints back and forth after drilling procedures. Casts were discarded in favor of early motion not just after cartilage repairs, but after all forms of ligament and tissue reconstruction.
In 1985 Richard Steadman, MD, popularized microfracturing cartilage injuries and athletes of all ages began seeking out this treatment. But by 1991, we had realized that microfractured cartilage often healed with scar tissue (rather than cartilage) and was not applicable to cases involving arthritis. We then understood that cartilage could heal, that cartilage cells could be replicated and that articular cartilage had unique signaling factors within its matrix. These growth and signaling factors in articular cartilage directed new bone marrow cells to form the unique cartilage structure. With this understanding, this author developed the articular cartilage paste graft (ACPG) technique. It had several components:
First, we noticed that the bigger the injury, the bigger the healing response. Small cartilage lesions that did not enter the bone marrow did not heal, while large fractures created a robust healing response.
Second, the intercondylar notch of the knee, after it was widened for an ACL reconstruction procedure, often healed back in. We surmised that if cartilage could regenerate there, it could also do so elsewhere and no harm would be done by harvesting a core of cartilage and bone from this location.
Third, we knew that the marrow cells (which were not yet called “stem” or “progenitor” cells), when encountering the articular cartilage matrix and stimulated by applied motion from a CPM machine, could form cartilage.
Finally, we knew that many arthritic cartilage lesions were irregular and diffuse and required a paste-like material to cover them effectively.
Eventually, in collaboration with Dr. Daniel Grande, we demonstrated that when a plug of articular cartilage and underlying bone is crushed into a paste, the cartilage cells increase their metabolic activity in trying to repair their own matrix. This effect (called upregulation) explained why the paste formed articular cartilage rather than scar tissue.
In collaboration with Dr. William Walsh, we demonstrated in sheep that the biomechanics of the paste graft repaired cartilage was superior to the tissue formed from microfracture alone.
Initial studies in humans with second-look biopsies revealed that approximately one-third of the arthritic knees that were repaired with paste grafting re-grew articular cartilage indistinguishable from normal. One-third were a mixture of fibrocartilage, and one-third developed only scar tissue.
Additionally, when asked how well the procedure relieved their pain, 90.2 % of patients reported good to excellent. When asked how well the procedure increased their ability to per- form regular activities, 92.7 % of patients reported good to excellent results, and 80.5 % of patients reported good to excellent return to heavy work or sports (as allowed). When asked how well the procedure met their expectations, 90.2 % of patients reported good to excellent and 90.2 % of patients reported probably yes or definitely yes that they would undergo the procedure again if needed.1
Interestingly, ACPG was not widely accepted as a dominant technique of cartilage repair. It was free (other than surgeon fees) and required no special instruments. Since any surgeon could be trained to do it, ACPG was available to developing world surgeons who had limited access to expensive devices. Yet because no commercial entity was promoting ACPG, it was not taught widely in corporate-sponsored surgeon education courses. Other techniques—such as plugs of intact cartilage and bone, matrices of collagen scaffolds, and cells grown in tissue culture then reinjected into the joint with open surgery—dominated the field. All of these were indicated only for isolated cartilage lesions and none for arthritis. None demonstrated better outcomes than ACPG.
To improve ACPG, the California Institute of Regenerative Medicine (CIRM) funded the Stone Research Foundation in collaboration with Dr. Anthony Ratcliffe to test, in multiple animal models, the addition of human stem cells to the paste graft construct. This work, now underway, has significant implications for veterinary and human injuries and disease. Many extremely expensive working and sports animals, especially dogs and horses, suffer cartilage injuries that end their careers. Similarly, millions of people suffer from sports injuries and arthritis which negatively affects their lives.
Additional studies with hydrogels and growth factors added to the paste graft technique are now being funded by donors to the public nonprofit Stone Research Foundation.
The development of novel cartilage repair models and the improvement of good existing techniques will have a dramatic impact on our goal of keeping people playing forever. As we say: Cancer may kill you, but arthritis ruins your life. It doesn’t have to.
1 Stone KR, Pelsis J, Na K, Walgenbach A, Turek T, et al. Articular cartilage paste graft for severe osteochondral lesions of the knee: a 10- to 23-year follow-up study. Knee Surg Sports Traumatol Arthroscopy 2017 Dec;25(12):3824-3833. doi: 10.1007/s00167-016-4323-7. Epub 2016 Oct 1.https://pubmed.ncbi.nlm.nih.gov/28209371

