Minding the Gap
There are two critical time gaps in joint injuries
The first is the interval from when a joint is injured to when arthritis sets in.The second is from when arthritis sets in to when you are considered old enough for artificial joint replacement surgery.
For the knee, shoulder and ankle injuries that I’ve treated, these gaps have ranged from years to decades. But as we move into the 21st century, those gaps are looking very different.
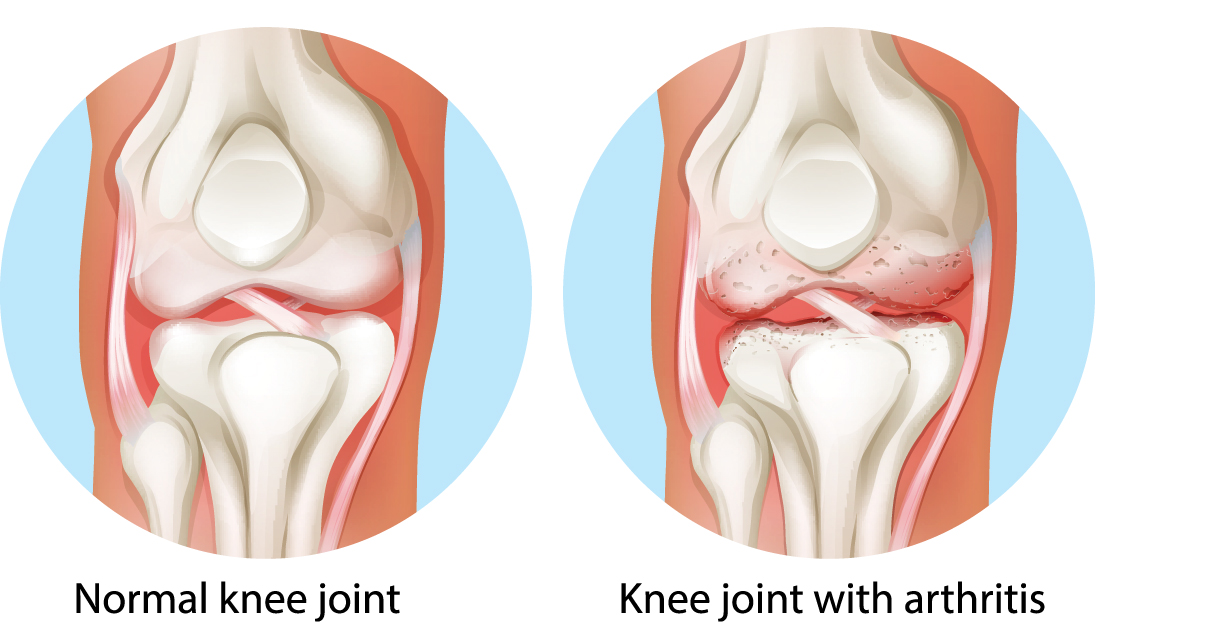
Let’s first look at them historically, starting with gap number one. In the past, when a significant cartilage injury occurred, the damaged cartilage was either ignored or removed. Those removal procedures—called meniscectomy for removing the knee joint meniscus, and chondroplasty for shaving away the articular cartilage—left the joints with poor shock absorption. The remaining cartilage surfaces wore out quickly, deforming the underlying bone. This in turn stimulated the formation of osteophytes (bone spurs), leading to instability of the joint. This was especially true when key ligaments (such as the ACL in the knee joint) were also torn, leading to further degradation.
Arthritis—the wearing away of the cartilage and the deformation of the underlying bone—occurred almost universally after cartilage was removed. The gap in time before arthritis set in was often silent. Many people, especially pro athletes, assumed they were healed, and returned to high levels of impact sports. Not until late in their careers did they realize they were faced with decades of joint pain.
The second gap is the time between when the arthritis has become symptomatic—with pain and loss of range of motion of the joint—and the time at which joint replacement is recommended. Joint replacements are generally not advised before the age of 65 because (a) they only last a couple of decades, (b) they are nonreversible, and (c) up to 50% of patients with full knee joint replacements still have pain ten years later. Patients were therefore told to rest their knees, limit their activities, lose weight and take arthritis pain medications until they were 65.Tough advice for a 30 year old former pro athlete, or even for an active weekend warrior!

Today, we can “mind the gaps” differently. There is excellent long-term data suggesting that when the joints are injured, repairing or replacing the missing cartilage in combination with stabilizing the damaged ligaments returns many people to active sports. This is achieved with less pain and better function scores, and without accelerating arthritis formation. Ten to 20-year outcome studies now show that current cartilage replacement techniques, such as meniscus replacement and articular cartilage paste grafting, provide long-term relief both for healthy knees (when first injured) and for the arthritic knee. The arthritic knee is thus able to delay or even avoid artificial joint replacement for decades.
For the ankle and shoulder there is significantly less data, but individual patient experiences have been encouraging.Cartilage replacement for the hip, unfortunately, is not yet available.
So mind the gap! Don't delay repairing or replacing injured critical tissues. And don't just rest and wait. An active lifestyle promotes health and productivity. The science of biologic joint replacement is advancing rapidly, and now offers much better solutions than, "just live with it."
Dr Stone explains that the Joint injury could lead to chronic and disabling arthritis, and there are far better solutions than waiting years for that new knee.
References
Burbine, S., Weinstein, A., Reichmann, W., Rome, B., Collins, J., Katz, J., & Losina, E. (2011). Projecting the Future Public Health Impact of the Trend Toward Earlier Onset of Knee Osteoarthritis in the Past 20 Years. In American College of Rheumatology Annual Scientific Meeting. Chicago, IL.
Lawrence, R. C., Felson, D. T., Helmick, C. G., et al. (2008). Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis and Rheumatism, 58(1), 26-35. doi:10.1002/art.23176
Losina, E., Weinstein, A. M., Reichmann, W. M., et al. (2013). Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care and Research, 65(5), 703-711. doi:10.1002/acr.21898
Jevsevar, D. S., Brown, G. A., Jones, D. L., et al. (2013). The American Academy of Orthopaedic Surgeons evidence-based guideline on: treatment of osteoarthritis of the knee, 2nd edition. The Journal of Bone and Joint Surgery. American Volume, 95(20), 1885-6
Lynch, T. S., Patel, R. M., Benedick, A., Amin, N. H., Jones, M. H., & Miniaci, A. (2015).
Systematic review of autogenous osteochondral transplant outcomes. Arthroscopy, 31(4), 746-54. doi:10.1016/j.arthro.2014.11.018
Kim Le, T., Montejano, L. B., Cao, Z., Zhao, Y., & Ang, D. (2012). Health care
