Discoid Meniscus
The meniscus cartilage, which is the critical shock absorber in the knee, is sometimes deformed at birth and causes problems later in life. Instead of being C-shaped, the central part of the meniscus is filled in with tissue. The problems associated with this condition, called discoid meniscus, can be significant.
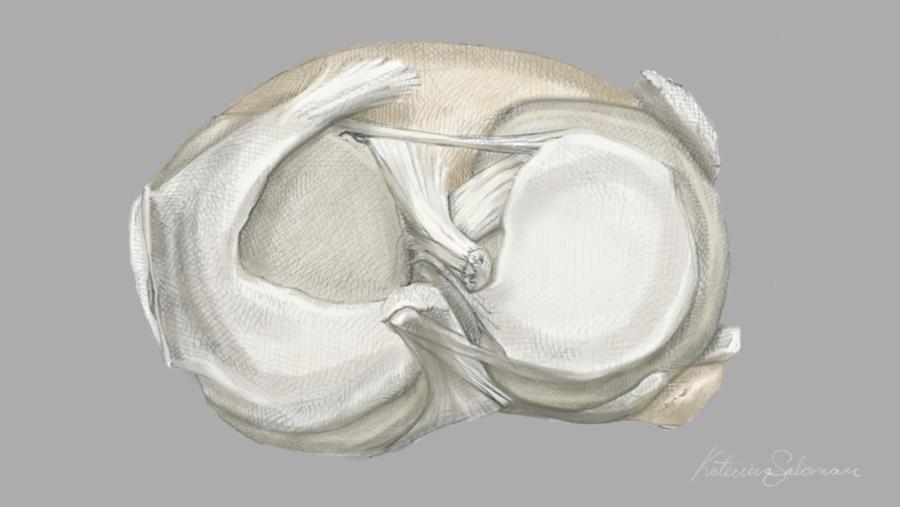
Original illustrated artwork by: Katerina Salsman
A normal meniscus is divided into two parts: the medial and the lateral semilunar cartilages. These are made of fibrous collagen tissue interspersed with several types of cells, including stem cells, and have a rich source of charged sugars (glycosaminoglycans) that are partly responsible for the mechanical properties of the tissue. This combination of crosslinked fibers and charged molecules absorbs and releases synovial fluid with each step, protecting the collagen structure of the meniscus. As you age, these crosslinks and sugars change—causing the tissue to become more brittle, less force diffusing, and more likely to degenerate or tear.
In the discoid meniscus, both the shape and the collagen are abnormal. Catching, popping, or locking in the knee are usually the symptoms the patient reports. When a well-meaning surgeon enters the knee and tries to trim back the meniscus to “saucerize” it back to a more familiar shape, too often the knee does poorly. The answer to why simply reshaping an abnormal meniscus is not enough is now clear: The entire structure is mis-constructed. The collagen throughout the center and the rim are abnormal, and thus the interactions between the collagen and the charged sugars are dysfunctional.
Efforts to regrow a normal meniscus in place of the deformed one have failed, probably due to the abnormal genetics responsible for tissue growth in that area. The only current solution for failed discoid meniscus treatments is complete meniscus replacement with a donor allograft. This has worked well in our hands over the past thirty years, but a question comes up: As the recipient’s cells migrate into the donor tissue do they stimulate normal tissue remodeling or is the collagen still abnormal? Meaning: does the new donor meniscus tissue integrate into the biology of the knee to form a “normal” meniscus. Would adding injections of growth factors or cytokines, to induce the body’s stem cell-derived self-repair cells to migrate into the tissue, make a difference? What is the potential of these regenerative injections, which provide promising results in other areas of joint treatment, in stimulating a cellular response to promote collagen formation?
The answers are not yet in, since not enough of the tissues we have transplanted since 1995 have failed over time for us to extract them and study the collagen. So, for now, the answer to the failed discoid meniscus is to replace it—before the knee becomes arthritic from the lack of its shock absorber.
The satisfying and exciting part of medicine and surgery is that the science is still so young, the questions so many, and the answers evolving.

